Editor’s Note:
The 18th World Conference of Lung Cancer (WCLC), hosted by International Association for the Study of Lung Cancer (IASLC), was held from October 15th–18th in Yokohama, Japan. It’s our great pleasure to have a brief interview with Prof. Silvia Novello.
Prof. Silvia Novello: our job—a choice of life that has to be renewed every day
Expert introduction
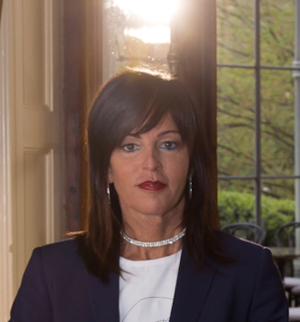
Professor Novello, MD, PhD (Figure 1), graduated in Medicine at the University of Turin, Italy in 1995. She then did a Postgraduate Course in Respiratory Medicine which she completed in 1999 summa cum laude. In 2006 she achieved a PhD in Human Oncology and went on doing a postgraduate in Medical Oncology in 2010.
Professor Novello is presently Professor of Medical Oncology at the Department of Oncology of the University of Turin, Italy.
Her previous positions include: Fellow at S. Luigi Hospital, Clinic of Respiratory Diseases, Orbassano, Turin, from 1995 to 1999 and Clinical Fellow at the same hospital, Thoracic Oncology DH, from 1999 to 2000. From 2000 to 2001 she was Resident A at the Institut Gustave Roussy, Villejuif, France. From 2001 to 2003, Research Fellow in the Medical Experimental and Clinical Sciences area at the Thoracic Oncology Division (University of Turin), and attending Physician at the Thoracic Oncology Division, from 2004 to 2010.
Professor Novello was also Thoracic Oncology Division tutor of Educational Classes in Thoracic Oncology and Educational Classes supported by AIPO (Hospital Pulmonologist Italian Association) for Specialised Doctors in Respiratory Diseases, Thoracic Surgery and Medical Oncology.
Interview
TLCR: We understand you are a world-recognized leader in the field of thoracic oncology, specially in the treatment of mesothelioma. How do you think to choose treatment strategy for malignant pleural mesothelioma? What is the best option from your perspective?
Mesothelioma is considered to be a relatively rare tumor, therapeutic alternatives are few and, unfortunately, only marginally effective with a standard approach only in first line for advanced disease. The choice of the best treatment strategy takes into consideration different factors: tumor and disease-related characteristics (tumor burden, presence of metastases), patient-related factors (performance status, co-morbidity), treatment related factors (toxicity, schedules of administration). A multidisciplinary management in centers mainly dedicated to this disease is important to define the initial diagnostic workup and the best treatment strategy with the contribution, if indicated, of surgery and radiotherapy.
Today the anti-folate/platinum doublet is the only systemic treatment approved but long-term survival remains an unmet goal. Innovative treatment alternatives have been explored and the addition of antiangiogenic compound to this standard treatment demonstrated encouraging results. Immunotherapy recently showed interesting results in this setting of patients but data have to be further confirmed.
Patients should be recommended to join clinical studies if possible. Scientific and clinical investigations, collaborative research across various institutions remain the basis of auspicable future changes.
TLCR: What do you think about the role of adjuvant TKI as adjuvant therapy in completely resected NSCLC? After the results of ADJUVANT trials being launched, what should researchers do to explore the best option for EGFR-sensitizing mutation patients?
Randomized trials have shown that patients with advanced NSCLC who are positive for activating EGFR mutations derive greater clinical benefit from EGFR tyrosine kinase inhibitors compared to standard front-line chemotherapy. There is a clear interest in evaluation of these drugs as adjuvant therapy and retrospective analysis has suggested possible clinical benefits. However, as yet, there are no conclusive prospective data to support the use of TKIs in this setting. Some studies as RADIANT or BR19 failed to demonstrate a disease-free survival or survival advantage with the use of adjuvant TKIs. On the other hand, new results lead to rethink of adjuvant therapy reporting a remarkable difference in disease-free survival, but data on overall survival are yet immature and the results are limited by a small sample size. Therefore, the available data do not support the use of TKIs as standard of care in completely resected, early-stage lung cancer. Several trials are ongoing so patients who respect all the required criteria should be included in order to obtain stronger evidences about the survival benefit, the optimal duration of treatment and eventually the financial burden resulting from this change.
TLCR: How do you design a control group in a clinical trial? As you know, it is helpful to draw a wonderful conclusion if you set an inefficient treatment as a control group, but it seems to be an unethical practice for the recruited participants. What is your opinion?
Clinical trials represent the key for drug development and for improving patients’ outcomes. These are the real basis to understand the risks and benefits of a treatment in a specific intended population. In every comparison trial the choice of the control group is crucial for the success of the study. The control arm has to be the standard of care for that investigated subset of patients. A study design of this type encourages trial accrual, allows the patients to access to investigational drugs and create results that are strong, generalizable and potentially practice-changing. That’s the way in which clinical trial may become a process of integrating scientific findings into clinical practice in a safe, systematic and ethical manner.
TLCR: Along the way to be an excellent researcher, would you like to share with us any stories behind? What encourage you to choose the career/field ( Figure 2 )?

Our job is a choice of life that has to be renewed every day. The support of this perspective is given by our patients, their faces and their hopes. Over the past two decades there have been substantial changes in the treatment of lung cancer but they are still not enough. Research is the only way to overcome limits and clinical trials represent the weapon we have in our daily medical activity. Clear words, precise explanations let patients understand the advantages of the inclusion in a clinical trial without feeling like a test case. The possibility to access promising new molecules and to offer valid therapeutic alternatives is very important and allows us to see long clinical histories, often much longer than we could expect.
I will never forget many patients and among them, Teresa, a never-smoker 56 years old woman affected by advanced lung adenocarcinoma (diagnosis on pleural effusion in September 2011). Her clinical conditions were excellent, she only complained of dyspnea with moderate exertion that didn’t limit her daily activities: she loved walking and visiting painting exhibitions with her husband. After the communication of the diagnosis she asked to start the therapy immediately. Unfortunately, the material was insufficient for molecular investigations. We decided to delay the start of the treatment and submit the patient to a new biopsy for molecular analysis. We needed many words and time to share the rational of the choice to the patient who was in a great understandable anxiety and was so frightened by further invasive measures. Finally, a fiberoptic bronchoscopy was performed and EML4-ALK resulted rearranged. Our patient received crizotinib in a clinical trial, chemotherapy as second line and after the further progression of disease was included in another study receiving ceritinib with good clinical and radiological response. Teresa was subjected to encephalic local treatment at the moment of oligoprogression with concomitant molecular analysis of the tissue and study of mutation profiles of resistance. Today Teresa assumes her tablets of brigatinib as fourth line of treatment. Her performance status is still good. Almost every time in day hospital she remembers her past days: the time spent for molecular analysis, all the procedures required to be included in clinical trials, the need of local treatment when the oral therapy didn’t seem enough anymore. But today she says it was worth it, she says that she finally understands the importance to take the time required to guide the choice of treatment and the big opportunity to access to investigational drugs through clinical trials.
These little daily successes remind us that change is possible and the way to pursue it is made of teamwork, passion and never stopping research.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
(Science Editor: Nikki Ling, TLCR, editor@tlcr.org)