RET-targeting molecular stratified non-small-cell lung cancers
Cancer genomics studies involving next generation sequencing (NGS) technology have successfully characterized therapeutic targets of lung cancer. Among lung adenocarcinoma genomes, activating mutations in EGFR, ERBB2, KRAS and BRAF as well as gene fusions of ALK, the products of which activate the autonomous proliferation of cancer cells via the Ras-MAPK pathway, have been regarded as so-called “driver mutations” (1). It is also known that these alterations exist in a mutually exclusive manner. In addition to these well-characterized driver mutations, independent groups from Japan, Korea and the USA recently found novel chromosome ten inversions that produce fusion genes containing the receptor tyrosine kinase encoding gene RET (2-5). Three of four groups applied NGS to determine the fusion genes. Kohno et al. and Ju et al. used cDNA samples from known driver-negative lung adenocarcinoma specimens for whole transcriptome sequencing to screen novel fusion gene products (2,3). Lipson et al. designed a custom target capture genomic DNA sequencing panel targeting the exons and introns of genes encoding previously reported cancer-related kinases and screened lung and colorectal cancer genomes (5).
By using different strategies, these groups identified the same KIF5B-RET fusion gene. In these primary reports, the authors found that RET fusion gene products are aberrantly expressed in tumor cells. Exogenously overexpressed RET fusion kinases are constitutively active and have transforming activity. Multi-kinase inhibitors, which reportedly inhibit RET, effectively suppress the growth advantage and transforming activity of RET fusion kinases (3-5). Further screening of lung adenocarcinoma-derived cell lines found that LC/2-ad cells, which were established from a pleural effusion from a Japanese patient with lung adenocarcinoma, expressed a CCDC6-RET fusion gene (6,7). In addition to experiments with exogenously overexpressed fusion RET, vandetanib, a RET-inhibiting multi-kinase inhibitor, successfully inhibited downstream signals and exhibited significant anti-tumor effects in vitro and in vivo.
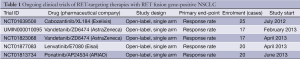
These findings strongly encourage the development of RET-targeted therapy for lung adenocarcinoma. Currently, five independent, open-label, single-arm, phase II studies have begun to assess the therapeutic effects of vandetanib (ZD6474), cabozantinib (XL184), lenvatinib (E7080) and ponatinib (AP24534) (Table 1). Drilon et al. reported promising results for the first three cases of their clinical trial, which investigated the efficacy of cabozantinib (8). In addition, a case report from Switzerland reported that vandetanib induced the remission of metastatic KIF5B-RET fusion gene-positive lung tumors (9). However, the infrequent prevalence of RET fusion gene-positive cases is a major obstacle hindering the further development of RET-targeted therapy. Primary and subsequent studies including a report by Wang et al. screened approximately 5,000 lung adenocarcinoma cases in total (10,11). RET fusion gene-positive cases were found in 1-2% of all non-small cell lung cancer (NSCLC) patients in Asian and European populations. Based on these estimations, more than 1,000 cases must be screened to identify 10 to 20 RET fusion gene-positive cases for proof-of-concept phase II studies. When efficacy is estimated with studies involving a larger number of cases, the number of pre-screening participants is also greater.
Full table
The clinicopathological features that characterize RET fusion gene-positive cases may help identify patients who should be subjected to further genetic screening. Most of the positive cases are adenocarcinomas, but several cases involve other histological types of NSCLC, such as adenosquamous carcinoma. The RET fusion is most likely to occur in young and/or never/light-smoker patients. Lung adenocarcinomas harboring KIF5B-RET fusions have well or moderately differentiated histological features similar to those harboring EGFR mutations, whereas lung adenocarcinomas harboring CCDC6-RET fusions often have signet-ring and mucinous cribriform features similar to EML4-ALK fusion-positive lung adenocarcinomas (10,11). These findings suggest a difficulty in distinguishing RET fusion gene-positive lung adenocarcinomas from commonly observed lung adenocarcinomas in Asian countries by histopathological diagnosis. Thus, appropriate genetic testing is mandatory for selecting RET fusion gene-positive cases.
Investigators have made much effort progress in recruiting adequate numbers of participants for prescreening for the above-mentioned phase II studies. The LURET (Lung Cancer with RET rearrangement) study, led by Dr. Koichi Goto at National Cancer Center Japan (UMIN00001009), evaluates the efficacy of vandetanib in 17 patients with RET fusion gene-positive NSCLC. The multi-kinase inhibiting spectrum of vandetanib includes EGFR, and VEGFR and RET. Although the therapeutic efficacy of vandetanib in advanced NSCLC patients was previously evaluated in “all-comer” clinical trials, significantly better therapeutic effects of vandetanib compared to pre-existing therapeutic regimens was not shown. We assume that another clinical trial recruiting only RET fusion gene-positive cases is necessary to evaluate the vandetanib effects. To recruit participants, a consortium designated LC-SCRUM (Lung Cancer Genomic Screening Project for Individualized Medicine in Japan) has been established. In LC-SCRUM, frozen biopsy tissues or pleural effusions from patients with non-squamous NSCLC without an EGFR mutation are curated from 136 hospitals throughout Japan, and RET fusion genes are detected using a combination of RT-PCR and FISH. Multiplex RT-PCR primers are designed to detect all of the previously described KIF5B-RET and CCDC6-RET variants. The positive cases are then subjected to break-apart and fusion FISH to validate the RT-PCR results. Cases positive by RT-PCR and FISH are eligible for the LURET study.
As Wang et al., mentioned in their report, standard methods for the detection of gene fusions, including RT-PCR, FISH and immunohistochemistry (IHC), have difficulty detecting RET fusion genes and their products (10). RT-PCR exhibits preferable sensitivity and specificity for detecting known fusion gene cDNA, but it is usually insufficient for detecting new partners or isoforms. Anti-RET antibodies that specifically distinguish overexpressed RET fusion proteins have not been generated. Although FISH is currently the most effective diagnostic technology for detecting chromosomal rearrangements, the high cost and need for technical expertise limit its practical application.
We should also take into account the cost efficiency of RET fusion gene detection, which only benefits the 1% of cases with a RET fusion gene. The detection of rare fusion genes is not just a pecuniary loss, it also wastes precious tissue samples obtained by biopsy or archived surgically resected specimens. To resolve these difficulties, genomic testing of lung adenocarcinoma driver mutations should evolve from single gene testing to multiplex genetic testing. Several technologies, including digital PCR and NGS-based target-capture sequencing, should be preferable candidates for future in vitro diagnostic systems. Although these technologies are still immature in their robustness and cost efficiency, these next-generation technologies must be positively applied to clinical diagnosis and may help in establishing a basis for the development of targeted therapy for lung cancer treatment.
Acknowledgements
Disclosure: The author declares no conflict of interest.
References
- Mitsudomi T, Suda K, Yatabe Y. Surgery for NSCLC in the era of personalized medicine. Nat Rev Clin Oncol 2013;10:235-44. [PubMed]
- Ju YS, Lee WC, Shin JY, et al. A transforming KIF5B and RET gene fusion in lung adenocarcinoma revealed from whole-genome and transcriptome sequencing. Genome Res 2012;22:436-45. [PubMed]
- Kohno T, Ichikawa H, Totoki Y, et al. KIF5B-RET fusions in lung adenocarcinoma. Nat Med 2012;18:375-7. [PubMed]
- Takeuchi K, Soda M, Togashi Y, et al. RET, ROS1 and ALK fusions in lung cancer. Nat Med 2012;18:378-81. [PubMed]
- Lipson D, Capelletti M, Yelensky R, et al. Identification of new ALK and RET gene fusions from colorectal and lung cancer biopsies. Nat Med 2012;18:382-4. [PubMed]
- Matsubara D, Kanai Y, Ishikawa S, et al. Identification of CCDC6-RET fusion in the human lung adenocarcinoma cell line, LC-2/ad. J Thorac Oncol 2012;7:1872-6. [PubMed]
- Suzuki M, Makinoshima H, Matsumoto S, et al. Identification of a lung adenocarcinoma cell line with CCDC6-RET fusion gene and the effect of RET inhibitors in vitro and in vivo. Cancer Sci 2013;104:896-903. [PubMed]
- Drilon A, Wang L, Hasanovic A, et al. Response to Cabozantinib in patients with RET fusion-positive lung adenocarcinomas. Cancer Discov 2013;3:630-5. [PubMed]
- Gautschi O, Zander T, Keller FA, et al. A patient with lung adenocarcinoma and RET fusion treated with vandetanib. J Thorac Oncol 2013;8:e43-4. [PubMed]
- Wang R, Hu H, Pan Y, et al. RET fusions define a unique molecular and clinicopathologic subtype of non-small-cell lung cancer. J Clin Oncol 2012;30:4352-9. [PubMed]
- Kohno T, Tsuta K, Tsuchihara K, et al. RET fusion gene: Translation to personalized lung cancer therapy. Cancer Sci 2013. [Epub ahead of print]. [PubMed]


