Improving the pathologic evaluation of lung cancer resection specimens
Lung cancer is the most common cause of cancer-related mortality worldwide and in the US; non-small cell lung cancer (NSCLC) represents approximately 85% of all cases (1,2). Despite improvements in methods of diagnosis and treatment, the aggregate overall 5-year survival rate of all patients with lung cancer has only improved from 12% in the 1970s to 17% in contemporary times (2). This is largely because most patients present with advanced disease for which curative therapy is currently unavailable. However, patients with early stage disease who undergo definitive surgery or combined modality therapy may have long term survival. The most effective current prognostic tool is the Tumor, Node, and Metastasis (TNM) staging system which is currently in its 7th edition (3).
Staging, while of great prognostic value, is only as useful as the degree of thoroughness with which it is applied (4,5). Comparison of clinical and pathological (post-resection) staging survival curves on the same patients reveals greater separation between the pN0-3 subsets than the cN subsets, in part because pathologic staging defines a group of pN0 tumors with better survival and a group of pN3 tumors with worse survival than predicted by clinical staging alone (6). This reflects the fact that clinical staging tests have sensitivity and specificity limitations that impair their accuracy (7-9).
Pathologic nodal stage is the most important determinant of prognosis in patients who undergo resection for NSCLC, with survival ranging from 56% in patients with pN0 to 6% in pN3 (6). It is also the main driver of post-operative management. For example, patients with pN1-3 disease benefit from adjuvant chemotherapy (10-12), while those with mediastinal lymph node metastasis may benefit from radiation therapy in addition to chemotherapy (13). However, pN-stage is the TNM category most susceptible to variability in both surgical resection techniques and pathologic evaluation (14).
Examination of large databases, such as the California Cancer Registry, the Surveillance, Epidemiology, and End Results (SEER) database and the National Cancer Data Base (NCDB), reveals worrisome statistics about pathologic nodal staging of NSCLC: a median of five lymph nodes are examined in pN0 resection specimens (15); 12% of all resections (and 18% of all ‘node-negative resections’) have no lymph nodes examined (pathologic NX) (14-17); 12% of pN0 cases have no N1 lymph nodes examined (18); and 42% of resections (and 62% of ‘mediastinal lymph node negative’ cases) have no mediastinal lymph nodes examined (14,15,19,20).
Less than fastidious pathologic nodal staging has profound survival implications. For example, survival of patients with pN0 disease rises sequentially with the number of lymph nodes examined, until a maximal improvement is achieved at approximately 18-20 lymph nodes, suggesting the impact of sampling error when few lymph nodes are examined (21,22); patients who undergo pNX resections have a significantly worse survival than those with pN0, much more akin to the survival of those with pN1 disease (17); and failure to examine mediastinal lymph nodes is associated with a 14% survival deficit (20). Even in patients in whom lymph node metastasis is detected, examination of all available lymph nodes remains of prognostic value. As with many cancers, including colorectal, esophageal and gastric cancer, the prognosis of NSCLC worsens with increasing number of lymph node metastasis or a rising positive lymph node ratio (23-29). The number of N1 lymph node metastases is independently prognostic (30), but also correlates strongly with the likelihood of mediastinal lymph node metastasis (23).
Accurate pathologic lymph node staging involves three key processes: the intra-operative collection of the hilar (station 10) and mediastinal (stations 2-9) nodes; secure transfer, and accurate communication of the anatomic provenance, of all specimens between the operating room and pathology laboratory; and examination of all delivered specimens in the pathology laboratory, including the intrapulmonary lymph nodes (stations 11-14) retrieved by gross dissection of the lung resection specimen. The collection of hilar and mediastinal lymph nodes is the responsibility of the operating surgeon, without whose performance those specimens cannot be obtained; the extraction of intrapulmonary lymph nodes and the examination of all provided specimens is the responsibility of the pathologist; and the delivery of specimens in a secure, anatomically distinguishable fashion is the joint responsibility of the operating room and pathology teams.
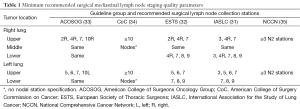
Multiple efforts have been made to standardize the extent of the surgical lymph node harvest (31-35). Although the details differ slightly, it is generally agreed that a systematic collection of hilar and mediastinal lymph nodes should be attempted by the surgeon (Table 1). Some further advocate that the surgeon should collect stations 11 (interlobar) and 12 (lobar) lymph nodes (33). On the pathology side, standard recommendations call for examination of all lymph nodes in the resection specimen (36). While pathologists routinely examine all specifically identified specimens, retrieval of intrapulmonary nodes is dependent on the quality of the gross dissection of the resection specimen, warranting careful oversight of this aspect of the pathology examination.
Full table
Although techniques for gross dissection of intrapulmonary lymph nodes have been described, actual practice likely varies significantly, as evidenced by the fact that almost 50% of pNX cases are lobectomy or greater resections, suggesting that not only were hilar and mediastinal lymph nodes not provided from the operating room, but intrapulmonary lymph nodes were not retrieved during gross dissection of the resection specimen (17,37-40). More direct evidence comes from a study in which fastidious re-examination of discarded remnant lung resection specimens revealed a median of four N1 lymph nodes examined and a median of six discarded. Furthermore, 29% of patients in this study had discarded lymph nodes with metastasis, and 12% of pN0 specimens had discarded N1 lymph node metastasis (41).
The pathology examination ideally should indicate the anatomic source of each of the lymph nodes examined (lymph node mapping) in order to provide clinicians a clear idea of whether lymph nodes are from N1, N2 or N3 stations. Because pathologists cannot identify the origin of lymph nodes provided by surgeons without accurate labeling, it is important for the communication between the operating room and the pathology laboratory to include unambiguous information on the source of all submitted specimens. The importance of this point is illustrated by an audit of mediastinal lymph node examination practices in a city-wide lung resection database, which revealed a 61% discordance between the procedure reported in operating surgeons’ notes and the procedure determined from objective review of the pathology report using pre-specified criteria. Whereas operating surgeons claimed a systematic nodal dissection in 45% of cases, only 8% met pathology criteria for systematic nodal dissection (42).
However, a blinded independent surgical review of the narrative description of the operation indicated that 30% of resections had adequately described a systematic nodal dissection (42). This sharp discordance between the operation narrative and the pathology report, which has been described as a ‘Tower of Babel’, suggests a multifaceted etiology of poor lymph node staging, encompassing actions both in the operating room and the pathology laboratory (43). This especially highlights the need for secure specimen delivery and better communication between the operating room and the pathology laboratory (42,44). A follow-up study in the same community institutions revealed marked improvement in concordance rate to 80% when surgeons used a lymph node specimen collection kit and checklist (45).
These observations suggest certain opportunities for intervention. The surgical hilar and mediastinal lymphadenectomy can be significantly improved with the use of pre-labelled surgical specimen collection kits, which help remind surgeons of the recommended lymph node collection procedure, provide a vehicle for the secure transfer of lymph node specimens, and with station-specific pre-labeling, eliminate all ambiguity about the anatomic source of each specimen. Use of such a specimen collection kit significantly improved hilar and mediastinal lymph node staging in a pilot study, with the ultimate result of an increase in the detection of pN2 disease from 8% of controls to 18% of cases (46). Routine use of kits such as these can address the operating room and communication aspects of the lymph node staging problem.
The finding of a high number of un-retrieved intrapulmonary lymph nodes has led to efforts to develop a more thorough standardized gross dissection method. Such a dissection protocol must be easy to learn, reproducible, quick to execute and feasible for use on fresh resection specimens in order not to interrupt the work flow in busy anatomic pathology laboratories. Such a protocol, in which blunt dissection of lymph nodes in the peri-bronchus is performed starting from the hilar surface of the resection specimen and working towards the periphery, has been shown to be feasible (47). This technique is easily taught, can be carried out on fresh specimens, requires a median of 9 minutes, and yields significantly more N1 lymph nodes than the current routine dissection protocol.
The combined use of the surgical specimen collection kit and thorough intrapulmonary lymph node retrieval protocols increased the number of lymph nodes examined in lung resection specimens from a median of 5 to 18, eliminated the pNX phenomenon, and, most importantly, increased the proportion of patients with detected node positive disease (and therefore potentially benefited by life-saving post-operative adjuvant therapy) from 30% to 45% (48). The potential survival impact of these combined interventions is large. Additionally, the improvement in lymph node mapping allows easy identification and correction of any errors in stage attribution.
In addition to identifying more patients with lymph node metastases, more lymph nodes with metastasis are found per patient with ‘node-positive disease’, potentially facilitating definitive examination of the prognostic impact of a higher number of lymph node metastasis in NSCLC. Ultimately, it is hoped that thorough lymph node retrieval will facilitate the search for other prognostic factors such as the real prevalence and prognostic value of micro-metastatic lymph node disease (detected by immunohistochemical analysis) and prognostic/predictive gene/protein expression patterns in primary tumors (49-54).
The combination of these two interventions, the surgical specimen collection kit and the standardized lung specimen dissection protocol, will be the subject of the ‘Strategies to Improve Lymph node Examination in Non-small cell lung cancer Trial’, an institutional randomization study with the acronym ‘SILENT’, which is currently in development. Objectives of this study are to test the impact of improved lymph node examination on stage distribution and survival, as well as the economic value associated with these corrective interventions.
Looking ahead, it is ultimately expected that molecular predictors of response to adjuvant therapy and independent molecular prognosticators can be identified from gene and protein expression profiles of primary tumors. However, optimal development and testing of such molecular markers will need accurately staged groups of patients (55,56). This will require marked improvement in the routine pathologic staging of resected lung cancer, to minimize the confounding of results caused by suboptimal use of the TNM staging system.
Major questions remain. How can we equitably compensate pathologists for any additional time, manpower, equipment and supply costs required to achieve more thorough examination? How can we successfully implement better pathology practices across the spectrum of practice environments? The first steps, possibly, are to universally acknowledge the existence of the gap in quality of pathologic staging, recognize the impact on survival, and commit to implementing corrective measures. Some measures, such as routine use of specimen collection kits, may be relatively easy to implement, while others might seem less so. Although improving the dissection and retrieval of intrapulmonary lymph nodes may require a bit more time and effort from pathologists, doing so will allow for more accurate identification of high-risk patients who will benefit from intensive post-operative intervention. This, in turn, is likely to provide a population-wide improvement in outcomes of resected early stage NSCLC.
Acknowledgements
Funding: Dr. Osarogiagbon was supported by a grant from the US National Institutes of Health: RO1 CA172253.
Footnote
Conflicts of Interest: Dr. Osarogiagbon has a patent application for a surgical specimen collection kit under review. All other authors have no conflicts of interest to declare.
References
- Jemal A, Center MM, DeSantis C, et al. Global patterns of cancer incidence and mortality rates and trends. Cancer Epidemiol Biomarkers Prev 2010;19:1893-907. [PubMed]
- Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin 2012;62:10-29. [PubMed]
- Part IV, Thorax. In: Edge S, Byrd DR, Compton CC, et al. editors. AJCC Cancer Staging Handbook. 7th ed. New York: Springer, 2010:297-323.
- Gajra A, Newman N, Gamble GP, et al. Effect of number of lymph nodes sampled on outcome in patients with stage I non-small-cell lung cancer. J Clin Oncol 2003;21:1029-34. [PubMed]
- Detterbeck F, Puchalski J, Rubinowitz A, et al. Classification of the thoroughness of mediastinal staging of lung cancer. Chest 2010;137:436-42. [PubMed]
- Rusch VW, Crowley J, Giroux DJ, et al. The IASLC Lung Cancer Staging Project: proposals for the revision of the N descriptors in the forthcoming seventh edition of the TNM classification for lung cancer. J Thorac Oncol 2007;2:603-12.
- Poncelet AJ, Lonneux M, Coche E, et al. PET-FDG scan enhances but does not replace preoperative surgical staging in non-small cell lung carcinoma. Eur J Cardiothorac Surg 2001;20:468-74; discussion 474-5. [PubMed]
- D’Cunha J, Herndon JE 2nd, Herzan DL, et al. Poor correspondence between clinical and pathologic staging in stage 1 non-small cell lung cancer: results from CALGB 9761, a prospective trial. Lung Cancer 2005;48:241-6. [PubMed]
- Annema JT, van Meerbeeck JP, Rintoul RC, et al. Mediastinoscopy vs endosonography for mediastinal nodal staging of lung cancer: a randomized trial. JAMA 2010;304:2245-52. [PubMed]
- Arriagada R, Bergman B, Dunant A, et al. Cisplatin-based adjuvant chemotherapy in patients with completely resected non-small-cell lung cancer. N Engl J Med 2004;350:351-60. [PubMed]
- Winton T, Livingston R, Johnson D, et al. Vinorelbine plus cisplatin vs. observation in resected non-small-cell lung cancer. N Engl J Med 2005;352:2589-97. [PubMed]
- Pignon JP, Tribodet H, Scagliotti GV, et al. Lung adjuvant cisplatin evaluation: a pooled analysis by the LACE Collaborative Group. J Clin Oncol 2008;26:3552-9. [PubMed]
- Lally BE, Zelterman D, Colasanto JM, et al. Postoperative radiotherapy for stage II or III non-small-cell lung cancer using the surveillance, epidemiology, and end results database. J Clin Oncol 2006;24:2998-3006. [PubMed]
- Allen JW, Farooq A, O’Brien TF, et al. Quality of surgical resection for nonsmall cell lung cancer in a US metropolitan area. Cancer 2011;117:134-42. [PubMed]
- Varlotto JM, Recht A, Nikolov M, et al. Extent of lymphadenectomy and outcome for patients with stage I nonsmall cell lung cancer. Cancer 2009;115:851-8. [PubMed]
- Ou SH, Zell JA. Prognostic significance of the number of lymph nodes removed at lobectomy in stage IA non-small cell lung cancer. J Thorac Oncol 2008;3:880-6. [PubMed]
- Osarogiagbon RU, Yu X. Nonexamination of lymph nodes and survival after resection of non-small cell lung cancer. Ann Thorac Surg 2013;96:1178-89. [PubMed]
- Osarogiagbon RU, Allen JW, Farooq A, et al. Pathologic lymph node staging practice and stage-predicted survival after resection of lung cancer. Ann Thorac Surg 2011;91:1486-92. Erratum in Ann Thorac Surg 2011;92:1556. [PubMed]
- Little AG, Rusch VW, Bonner JA, et al. Patterns of surgical care of lung cancer patients. Ann Thorac Surg 2005;80:2051-6; discussion 2056. [PubMed]
- Osarogiagbon RU, Yu X. Mediastinal lymph node examination and survival in resected early-stage non-small-cell lung cancer in the surveillance, epidemiology, and end results database. J Thorac Oncol 2012;7:1798-806. [PubMed]
- Ludwig MS, Goodman M, Miller DL, et al. Postoperative survival and the number of lymph nodes sampled during resection of node-negative non-small cell lung cancer. Chest 2005;128:1545-50. [PubMed]
- Osarogiagbon RU, Ogbata O, Yu X. Number of lymph nodes associated with maximal reduction of long-term mortality risk in pathologic node-negative non-small cell lung cancer. Ann Thorac Surg 2014;97:385-93. [PubMed]
- Fukui T, Mori S, Yokoi K, et al. Significance of the number of positive lymph nodes in resected non-small cell lung cancer. J Thorac Oncol 2006;1:120-5. [PubMed]
- Lee JG, Lee CY, Park IK, et al. Number of metastatic lymph nodes in resected non-small cell lung cancer predicts patient survival. Ann Thorac Surg 2008;85:211-5. [PubMed]
- Wei S, Asamura H, Kawachi R, et al. Which is the better prognostic factor for resected non-small cell lung cancer: the number of metastatic lymph nodes or the currently used nodal stage classification? J Thorac Oncol 2011;6:310-8. [PubMed]
- Rusch VW, Giroux DJ. Nodal staging in lung cancer: lymph node location or number? J Thorac Oncol 2011;6:237-8. [PubMed]
- Jonnalagadda S, Arcinega J, Smith C, et al. Validation of the lymph node ratio as a prognostic factor in patients with N1 nonsmall cell lung cancer. Cancer 2011;117:4724-31. [PubMed]
- Nwogu CE, Groman A, Fahey D, et al. Number of lymph nodes and metastatic lymph node ratio are associated with survival in lung cancer. Ann Thorac Surg 2012;93:1614-9; discussion 1619-20. [PubMed]
- Taylor MD, Lapar DJ, Thomas CJ, et al. Lymph node ratio predicts recurrence and survival after R0 resection for non-small cell lung cancer. Ann Thorac Surg 2013;96:1163-70. [PubMed]
- Jonnalagadda S, Smith C, Mhango G, et al. The number of lymph node metastases as a prognostic factor in patients with N1 non-small cell lung cancer. Chest 2011;140:433-40. [PubMed]
- Rami-Porta R, Wittekind C, Goldstraw P, et al. Complete resection in lung cancer surgery: proposed definition. Lung Cancer 2005;49:25-33. [PubMed]
- Lardinois D, De Leyn P, Van Schil P, et al. ESTS guidelines for intraoperative lymph node staging in non-small cell lung cancer. Eur J Cardiothorac Surg 2006;30:787-92. [PubMed]
- Darling GE, Allen MS, Decker PA, et al. Randomized trial of mediastinal lymph node sampling versus complete lymphadenectomy during pulmonary resection in the patient with N0 or N1 (less than hilar) non-small cell carcinoma: results of the American College of Surgery Oncology Group Z0030 Trial. J Thorac Cardiovasc Surg 2011;141:662-70. [PubMed]
- CoC Quality of Care Measures. Available online: https://www.facs.org/quality%20programs/cancer/ncdb/qualitymeasures, accessed on Jul 11, 2015.
- National Comprehensive Cancer Network Non-Small Cell Lung Cancer Guidelines version 2.2012. Principles of surgical therapy. Available online: http://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf, accessed on Oct 8, 2012.
- Association of Directors of Anatomic and Surgical Pathology. Recommendations for processing and reporting of lymph node specimens submitted for evaluation of metastatic disease. Am J Clin Pathol 2001;115:799-801. [PubMed]
- Gephardt GN, Baker PB. Lung carcinoma surgical pathology report adequacy: a College of American Pathologists Q-Probes study of over 8300 cases from 464 institutions. Arch Pathol Lab Med 1996;120:922-7. [PubMed]
- Lester SC. Manual of Surgical Pathology. 2nd ed. Philadelphia: Elsevier Churchill Livingstone, 2006:497-516.
- Westra WH, Hruban RH, Phelps TH, et al. editors. Surgical Pathology Dissection. 2nd ed. New York: Springer, 2002.
- Osarogiagbon RU, Allen JW, Farooq A, et al. Outcome of surgical resection for pathologic N0 and Nx non-small cell lung cancer. J Thorac Oncol 2010;5:191-6. [PubMed]
- Ramirez RA, Wang CG, Miller LE, et al. Incomplete intrapulmonary lymph node retrieval after routine pathologic examination of resected lung cancer. J Clin Oncol 2012;30:2823-8. [PubMed]
- Osarogiagbon RU, Allen JW, Farooq A, et al. Objective review of mediastinal lymph node examination in a lung cancer resection cohort. J Thorac Oncol 2012;7:390-6. [PubMed]
- Detterbeck FC. The fable of Babel and building a foundation for quality. J Thorac Oncol 2012;7:267-8. [PubMed]
- Makary MA, Epstein J, Pronovost PJ, et al. Surgical specimen identification errors: a new measure of quality in surgical care. Surgery 2007;141:450-5. [PubMed]
- Osarogiagbon RU, Sareen S, Eke R, et al. Audit of lymphadenectomy in lung cancer resections using a specimen collection kit and checklist. Ann Thorac Surg 2015;99:421-7. [PubMed]
- Osarogiagbon RU, Miller LE, Ramirez RA, et al. Use of a surgical specimen-collection kit to improve mediastinal lymph-node examination of resectable lung cancer. J Thorac Oncol 2012;7:1276-82. [PubMed]
- Osarogiagbon RU, Eke R, Sareen S, et al. The impact of a novel lung gross dissection protocol on intrapulmonary lymph node retrieval from lung cancer resection specimens. Ann Diagn Pathol 2014;18:220-6. [PubMed]
- Osarogiagbon RU, Ramirez RA, Wang CG, et al. Dual intervention to improve pathologic staging of resectable lung cancer. Ann Thorac Surg 2013;96:1975-81. [PubMed]
- Rusch VW, Hawes D, Decker PA, et al. Occult metastases in lymph nodes predict survival in resectable non-small-cell lung cancer: report of the ACOSOG Z0040 trial. J Clin Oncol 2011;29:4313-9. [PubMed]
- Chen HY, Yu SL, Chen CH, et al. A five-gene signature and clinical outcome in non-small-cell lung cancer. N Engl J Med 2007;356:11-20. [PubMed]
- Zhu CQ, Ding K, Strumpf D, et al. Prognostic and predictive gene signature for adjuvant chemotherapy in resected non-small-cell lung cancer. J Clin Oncol 2010;28:4417-24. [PubMed]
- Subramanian J, Simon R. Gene expression-based prognostic signatures in lung cancer: ready for clinical use? J Natl Cancer Inst 2010;102:464-74. [PubMed]
- Kratz JR, He J, Van Den Eeden SK, et al. A practical molecular assay to predict survival in resected non-squamous, non-small-cell lung cancer: development and international validation studies. Lancet 2012;379:823-32. [PubMed]
- Lu Y, Wang L, Liu P, et al. Gene-expression signature predicts postoperative recurrence in stage I non-small cell lung cancer patients. PLoS One 2012;7:e30880. [PubMed]
- Xie Y, Minna JD. Non-small-cell lung cancer mRNA expression signature predicting response to adjuvant chemotherapy. J Clin Oncol 2010;28:4404-7. [PubMed]
- Osarogiagbon RU. Predicting survival of patients with resectable non-small cell lung cancer: Beyond TNM. J Thorac Dis 2012;4:214-6. [PubMed]


