The TORCH trial
Non-small cell lung cancer (NSCLC) remains a major cause of cancer-related death worldwide (1). Unfortunately the majority of patients are diagnosed with advanced disease where the treatment intent is palliative. The mainstay of treatment, until recently, has been platinum based doublet chemotherapy which improves symptoms and prolongs survival compared to best supportive care (2). Increased interest in the molecular pathways which drive cancer growth has led to the development of targeted agents such as the epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs) erlotinib and gefitinib which are both approved for use in first-line for advanced NSCLC harbouring an EGFR activating mutation and as second- or third-line treatment (erlotinib) for advanced NSCLC, independently of the EGFR mutational status.
The TORCH trial was a randomised, non-inferiority, phase III trial comparing erlotinib given as first-line therapy followed by standard chemotherapy with cisplatin-gemcitabine versus the opposite standard sequence, in unselected advanced NSCLC patients (3).
The BR.21 trial had shown a survival advantage of erlotinib over best supportive care in an unselected group of patients with NSCLC who had failed at least one line of chemotherapy (4) whilst two phase II trials had provided further evidence of good response to erlotinib in the first line setting (5,6). The protocol was developed before information about predictive clinical factors for response to EGFR-TKIs such as being female, of East Asian origin, a non-smoker or having adenocarcinoma histology were known (7) and before evidence suggested that EGFR TKIs achieve better response rate (RR), progression-free survival (PFS) and quality of life when compared to chemotherapy in EGFR mutant patients (8). Based on this emerging information, EGFR mutation analysis of available tumours was performed retrospectively and unplanned interaction tests were also performed for EGFR mutation and all clinical factors which could have affected efficacy.
The trial aimed to recruit 900 patients with stage IIIB or IV NSCLC who were randomly assigned in a 1:1 ratio to the two treatment arms. Patients in the experimental arm received 150 mg of erlotinib daily until progression at which point they received cisplatin (80 mg/m2 on day 1) and gemcitabine (1,200 mg/m2 on day 1 and 8) for a maximum of 6 cycles. The standard arm received cisplatin and gemcitabine at the same doses and on progression was switched to erlotinib 150 mg daily. Imaging was performed after 3 and 6 cycles and thereafter 12 weekly. The primary endpoint for the trial was overall survival (OS). Secondary endpoints were total PFS, PFS after first line therapy (first-PFS), tumour response and toxicity. Non-inferiority was defined as the 95% confidence interval for the hazard ratio (HR) of death having an upper limit of 1.25. Two interim analyses were pre-planned after approximately 50% and 75% of the events occurred so that the trial would be stopped early if either the experimental arm was shown to be inferior to the standard arm or confirmed to be non-inferior to the standard arm.
The trial was stopped after the first planned interim analysis when 760 patients had been recruited. The analysis showed inferiority of the experimental arm, as it was far lower than the boundary limit of 0.583. Three hundred and eighty patients had been randomised to each arm. The median age of patients was 62 years old, 33.7% were women and approximately 50% of the patients were performance status 0. Only 3.2% of patients were East Asian and 20.5% were non-smokers. Over 55% of the patients recruited had adenocarcinoma histology. Clinical factors which could have influenced the likelihood of patients harbouring EGFR mutations such as East Asian origin and adenocarcinoma histology were well balanced between the two arms. The tumour tissue was analysed for EGFR mutational status in 36.2% of patients and 39 patients were found to have EGFR-mutation positive tumours. Twenty of these patients were randomised to the standard arm and 19 to the experimental arm.
In the standard arm, 371 patients received at least one cycle of cisplatin-gemcitabine chemotherapy with 5 being the median number of cycles received. Documented disease progression was confirmed in 316 patients of whom 28.5% did not receive second-line erlotinib. In the experimental arm, 373 patients received at least one dose of erlotinib, disease progression was documented in 333 patients and 41.7% of these patients did not receive second-line therapy. After 24.3 months median follow up, patients treated in the standard arm had longer first-PFS, PFS and OS (Table 1). EGFR wild type patients enrolled in the standard arm had longer PFS and OS whilst patients with EGFR mutations treated in the experimental arm had longer first-PFS but shorter PFS and OS (Table 2). It is important to point out that this is based on a maximum of 38 events in the two arms.
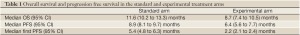
Full table

Full table
The TORCH trial convincingly demonstrates that, in an unselected group of patients with advanced NSCLC, chemotherapy remains the optimal choice for first-line treatment and supports the existing evidence (9) that patients with confirmed EGFR wild type tumours should receive chemotherapy as first-line treatment.
The potential benefits of EGFR TKIs in later lines of therapy for unselected populations as suggested by the BR.21 and SATURN trials (4,10) are not discounted by this trial but it does suggest their role in first-line treatment is limited. Notably, 28% of patients in the standard arm and over 41% in the experimental arm did not receive second-line therapy. This adds weight to the argument to consider maintenance therapy to improve outcomes in advanced NSCLC.
Significant effort in this trial was made on obtaining tissue samples for EGFR mutation testing with 36.2% of patient’s samples tested. This represents, along with the IPASS trial (9) the highest number of samples tested in a clinical trial in which there was not mandatory testing. Of the samples tested 14.2% of tumours harboured an EGFR mutation and this is consistent with the mutation rate previously reported in the western population (8). Amongst patients with EGFR mutated tumours the first line PFS was longer for those treated with first-line erlotinib consistent with the results of the IPASS, OPTIMAL, and EURTAC trials (9,11,12). Interestingly, OS was shorter in EGFR mutant patients treated with first-line erlotinib, this may be due to the small number of patients being dealt with or confounded by the crossover of therapies. However, the mature survival data from these trials also did not demonstrate a survival advantage for EGFR mutated patients receiving first line EGFR-TKI compared to chemotherapy, again likely due to the confounding effects of crossover (13,14).
The TORCH trial has confirmed the role of first-line chemotherapy in unselected populations and patients with EGFR wild type tumours and supports the use of erlotinib in patients with EGFR mutated tumours. Furthermore, this trial highlights the importance of ensuring sufficient biopsy material is available to perform genomic testing to define the best treatment strategy and the need for predictive biomarkers to be developed alongside targeted agents to ensure the potential benefits are not underestimated in the overall population.
The multicenter, double-blinded, placebo controlled, randomized phase III trial FASTACT-2 evaluated the efficacy of a sequential schedule of erlotinib with chemotherapy in unselected patients with advanced NSCLC (15). Four hundred and fifty one patients were randomized (1:1) to receive up to 6 cycles of gemcitabine (1,250 mg/m2 on d1 and 8) plus platinum (carboplatin AUC 5 or cisplatin 75 mg/m2 on d1) q4w, with either intercalated erlotinib (150 mg/day on d15-28) or placebo. Non-progressing patients were treated with maintenance placebo/erlotinib until progressive disease or intolerable toxicity. The trial met its primary endpoint showing longer PFS for the erlotinib arm [7.6 vs. 6.0 months, HR 0.57 (95% CI, 0.46-0.70); P<0.0001], confirmed by independent radiology review. The updated analysis showed longer OS for the erlotinib arm (18.3 vs. 15.2 months, HR 0.79, 95% CI, 0.64-0.99, P=0.0042) and notably 85% of the patients in the placebo arm received an EGFR-TKI as second-line (16). Two hundred and forty-one patients were tested for EGFR mutations and 97 patients were found to be EGFR mutant. The EGFR mutant subgroup treated with intercalated erlotinib achieved longer PFS (16.8 vs. 6.9 months, HR 0.25, P<0.0001) and OS (31.4 vs. 20.6 months, HR 0.48, P=0.0092) but in the EGFR wild type population there was no difference in PFS and OS between the arms. Patients receiving intercalated erlotinib did not experience unexpected toxicity and FASTACT-2 provides very interesting data on the sequence of chemotherapy and EGFR-TKIs in the EGFR mutant population.
Thanks to better understanding of molecular biology and oncogenic drivers, crizotinib is now standard of care for ALK mutant advanced NSCLC (17,18) and other new molecularly driven agents are on the pipeline. Hopefully, new discoveries will lead to increase in the number of treatment options for NSCLC and, for this reason, trials investigating the optimal sequence of therapies will be needed to define the best treatment strategy.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin 2011;61:69-90.
- Schiller JH, Harrington D, Belani CP, et al. Comparison of four chemotherapy regimens for advanced non-small-cell lung cancer. N Engl J Med 2002;346:92-8.
- Gridelli C, Ciardiello F, Gallo C, et al. First-Line Erlotinib Followed by Second-Line Cisplatin-Gemcitabine Chemotherapy in Advanced Non-Small-Cell Lung Cancer: The TORCH Randomized Trial. J Clin Oncol 2012;30:3002-11.
- Shepherd FA, Rodrigues Pereira J, Ciuleanu T, et al. Erlotinib in previously treated non-small-cell lung cancer. N Engl J Med 2005;353:123-32.
- Giaccone G, Gallegos Ruiz M, Le Chevalier T, et al. Erlotinib for frontline treatment of advanced non-small cell lung cancer: a phase II study. Clin Cancer Res 2006;12:6049-55.
- Jackman DM, Yeap BY, Lindeman NI, et al. Phase II clinical trial of chemotherapy-naive patients > or = 70 years of age treated with erlotinib for advanced non-small-cell lung cancer. J Clin Oncol 2007;25:760-6.
- Thatcher N, Chang A, Parikh P, et al. Gefitinib plus best supportive care in previously treated patients with refractory advanced non-small-cell lung cancer: results from a randomised, placebo-controlled, multicentre study (Iressa Survival Evaluation in Lung Cancer). Lancet 2005;366:1527-37.
- Rosell R, Moran T, Queralt C, et al. Screening for epidermal growth factor receptor mutations in lung cancer. N Engl J Med 2009;361:958-67.
- Mok TS, Wu YL, Thongprasert S, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med 2009;361:947-57.
- Cappuzzo F, Ciuleanu T, Stelmakh L, et al. Erlotinib as maintenance treatment in advanced non-small-cell lung cancer: a multicentre, randomised, placebo-controlled phase 3 study. Lancet Oncol 2010;11:521-9.
- Zhou C, Wu YL, Chen G, et al. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol 2011;12:735-42.
- Rosell R, Carcereny E, Gervais R, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol 2012;13:239-46.
- Fukuoka M, Wu YL, Thongprasert S, et al. Biomarker analyses and final overall survival results from a phase III, randomized, open-label, first-line study of gefitinib versus carboplatin/paclitaxel in clinically selected patients with advanced non-small-cell lung cancer in Asia (IPASS). J Clin Oncol 2011;29:2866-74.
- Zhou C, Wu YL, Liu X, et al. Overall survival (OS) results from OPTIMAL (CTONG0802), a phase III trial of erlotinib (E) versus carboplatin plus gemcitabine (GC) as first-line treatment for Chinese patients with EGFR mutation-positive advanced non-small cell lung cancer (NSCLC). J Clin Oncol 2012;30:abstr 7520.
- Mok T, Wu Y, Thongprasert S, et al. A randomized placebo-controlled phase III study of intercalated erlotinib with gemcitabine/platinum in first-line advanced non-small cell lung cancer (NSCLC): FASTACT-II. J Clin Oncol 2012;30:abstr 7519.
- Mok TS, Lee J, Zhang L, et al. Biomarker analyses and overall survival (OS) from the randomized, placebo-controlled, phase 3, FASTACT-2 study of intercalated erlotinib with first-line chemotherapy in advanced non-small-cell lung cancer (NSCLC). Annals of oncology: official journal of the European Society for Medical Oncology / ESMO. 2012;23:ix400-ix46.
- Kwak EL, Bang YJ, Camidge DR, et al. Anaplastic lymphoma kinase inhibition in non-small-cell lung cancer. N Engl J Med 2010;363:1693-703.
- Shaw AT, Kim DW, Nakagawa K, et al. Phase III study of crizotinib versus pemetrexed or docetaxel chemotherapy in patients with advanced ALK-positive non-small cell lung cancer (NSCLC) (PROFILE 1007). Presented at the 37th Congress of the European Society for Medical Oncology (ESMO), Vienna, Austria, 2012: Abstract LBA1.


