Spontaneous bilateral pneumothorax in a patient with metastatic synovial sarcoma while under chemotherapy
Abstract: We report a case of synovial sarcoma of the lower limbs with pulmonary metastasis in a 24-year-old male patient who developed progressive spontaneous bilateral pneumothorax while he was on chemotherapy. Chest tubes inserted and achieved recovery in the left side whereas the right side became worse. Right lung decortication was carried out and the biopsy confirmed the diagnosis of synovial sarcoma metastasis. Thereafter, the patient was kept on chemotherapy of IV ifosfamide + etoposide D1-5, and after 2 cycles he traveled back to his country to continue treatment there.
Key words: Sarcoma; pneumothorax; metastasis
Introduction
Soft tissue sarcomas (STS) are a relatively rare, heterogeneous group of tumors that arise from mesenchymal tissue. It is estimated 8,300 new cases of STS were diagnosed in the United States in 2002 (1). Synovial sarcoma is histologically well defined soft tissue tumor which is common among other soft tissue tumors constituting about 10% of cases, but in Qatar it accounts for less than 5% which may be explained by the small population of this country. Metastatic soft tissue sarcoma is often exclusively located in the lung. The appearance of spontaneous pneumothorax in metastatic lung disease, however, is rare and most commonly described in advanced disease or during cytotoxic therapy (2,3). In this report we present a case of synovial sarcoma which was metastasized to the lungs causing bilateral pneumothorax during chemotherapy. The aim of presenting this case was to highlight the importance of remembering this complication even if chemotherapy had been started.
Case report
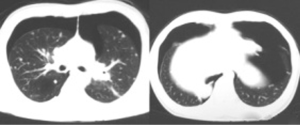
A 24-year-old male patient had poorly differentiated biphasic synovial sarcoma involving the soft tissue over the posterior aspect and postero-medial aspect of the right tibia since February 2007. Being metastatic (mainly to the lungs) he received six cycles of Doxorubicin and Ifosfamide D1 after which lung metastasis disappeared completely as evidenced by chest CT scan. One month later the primary paratibial synovial sarcoma was resected (limb saving) to decrease the bulk of the disease. The patient was given 2 additional cycles of same above chemotherapy, but because of reaching cumulative dose of doxorubicin (400 mg/m2), we shifted the patient later on to Ifosfamide + etoposide D1-5. Repeat chest CT showed bilateral pulmonary metastasis but this time with right-sided pleural effusion and mild left sided pneumothorax. We decided to give more cycles of chemotherapy. During the period of the last 2 cycles, the patient developed mild constant dry cough, which did not affect his performance at all but he denied shortness of breath or hemoptysis. Upon physical examination, the patient was not distressed with stable vital signs, but he had diminished breath sounds mainly over both lower zones with decreased auscultatory vocal fremitus. A follow up chest CT scan showed progression of the disease with bilateral spontaneous pneumothorax as shown in Figures 1,2. Consequently, the patient was admitted to Al-Amal hospital (oncology unit) and air aspiration tried to evacuate the pleural cavity by wide bore needle, but failed, thus, the patient was transferred to cardiothoracic department for close observation and continuity of care.
On the next day, chest tubes were inserted on both sides with under water seal air-evacuation and the patient. A follow up chest x-ray showed improved left side pneumothorax, whereas the right side became worse. Right lung decortication was carried out and the biopsy confirmed the diagnosis of synovial sarcoma metastasis. The patient was kept on the same chemotherapy (IV ifosfamide + etoposide D1-5), and after 2 cycles he traveled back to his country to continue treatment there.

Discussion
The time from presentation to development of pulmonary metastases is difficult to ascertain from the literature. In some reports, more than 75% of patients developed lung metastases within 1 year after presentation (4). In our patient there was metastasis at time of presentation and bilateral pneumothorax was developed six months later.
Several theories regarding possible mechanisms of pleural disruption in metastatic or primary lung disease have been put forward (2,5). Spontaneous rupture of necrotic tumor tissue or of oncological treatment may create bronchopleural fistulae. Alternatively, intermittent bronchiolar obstruction by nodules at the lung periphery may lead to subpleural blebs (5). Histological examination of the nodules excised in our second case revealed neither tumor necrosis nor blebs. It is possible that tumor invasion and disruption of the visceral pleura and of peripheral bronchioles might have produced slow air leakage resulting in a small and clinically silent pneumothorax.
The radiographic appearances of the pulmonary metastases from sarcoma was described in some reports. In general, these studies suggest that the pulmonary metastases present as solitary or multiple pulmonary nodules (6-8). In our patient metastasis appeared as multiple pulmonary nodules.
Treatment of such pneumothorax associated with lung cancer or lung metastasis may be difficult especially if the underlying mechanism is broncho-pleural fistula which could lead to persistent pneumothorax inspite of chest tube insertion which will mandates surgical intervention or chemical pleurodesis particularly in case of chemo-induced bilateral spontaneous pneumothorax and from the initial presentation.
Conclusions
The lesson taught from our case is not to approach from red lines which is represented in our case by the cumulative dose of doxorubicin as it is blamed to play role in the causation of pneumothorax in sarcoma cases.
Moreover, our case report and other similar reported cases suggests that spontaneous pneumothorax can complicate metastatic synovial sarcoma especially those with lung metastasis on first presentation or its treatment with either anthracycline or other chemotherapy, therefore we must have lower threshold or high degree of suspicion when facing a case of persistent cough in above susceptible groups of patients because sometimes we will have serious and even fatal consequences, which could be preventable from the beginning.
Acknowledgements
Disclosure: The author declares no conflict of interest.
References
- Jemal A, Thomas A, Murray T, et al. Cancer statistics, 2002. CA Cancer J Clin 2002;52:23-47.
- Furrer M, Althaus U, Ris HB. Spontaneous pneumothorax from radiographically occult metastatic sarcoma. Eur J Cardiothorac Surg 1997;11:1171-3.
- Upadya A, Amoateng-Adjepong Y, Haddad RG. Recurrent bilateral spontaneous pneumothorax complicating chemotherapy for metastatic sarcoma. South Med J 2003;96:821-3.
- Songür N, Dinç M, Ozdilekcan C, et al. Analysis of lung metastases in patients with primary extremity sarcoma. Sarcoma 2003;7:63-7.
- Wright FW. Spontaneous pneumothorax and pulmonary malignant disease--a syndrome sometimes associated with cavitating tumours. Report of nine new cases, four with metastases and five with primary bronchial tumours. Clin Radiol 1976;27:211-22.
- Pass HI, Dwyer A, Makuch R, et al. Detection of pulmonary metastases in patients with osteogenic and soft-tissue sarcomas: the superiority of CT scans compared with conventional linear tomograms using dynamic analysis. J Clin Oncol 1985;3:1261-5.
- Vanel D, Henry-Amar M, Lumbroso J, et al. Pulmonary evaluation of patients with osteosarcoma: roles of standard radiography, tomography, CT, scintigraphy, and tomoscintigraphy. AJR Am J Roentgenol 1984;143:519-23.
- Peuchot M, Libshitz HI. Pulmonary metastatic disease: radiologic-surgical correlation. Radiology 1987;164:719-22.