Overall survival in non-small cell lung cancer—what is clinically meaningful?
Non-small cell lung cancer (NSCLC; 80–85% of all lung cancers) continues to be one of the major causes of cancer-related deaths around the world (1). The development of molecularly targeted therapies (small molecules and monoclonal antibodies) has, however, significantly improved outcomes in the metastatic setting for NSCLC patients harbouring activated oncogenes such as EGFR and translocated ALK. By targeting the main pathways of NSCLC signal transduction, these drugs dramatically improved progression-free survival (PFS) and quality of life (QoL) in this highly selected subgroup of NSCLC patients sparing them from toxic chemotherapy approaches. However, for the vast majority of patients platinum-based chemotherapy remains the only potential treatment and has led to significantly improved survival outcomes with a “plateau” of about 10–11 months median survival (2). Subsequently, significant advances have been made with the introduction of pemetrexed, especially against the non-squamous cell subtype. The addition of this agent led to a further improvement in survival to 12–13 months (3) and up to 14 months with the introduction of maintenance therapy (4). Nonetheless, even with these therapies, the majority of patients with NSCLC do not attain prolonged disease control (5).
More recently, targeted therapies administered to patients selected by reliable and biologically relevant biomarkers (e.g., EGFR mutations, ALK rearrangement, PD-L1 expression) have produced substantial improvements in outcomes that have rapidly transformed patient care for several types of NSCLC (6). By improving the ability to identify the molecular drivers of cancer, it is anticipated that highly effective, molecularly targeted regimens will continue to be developed for usage in patients who can be identified prospectively as likely to benefit from treatment. In addition, newer treatment modalities such as immune therapies are emerging as highly effective therapies that are providing improvements in NSCLC patients outcomes far beyond what was achieved in the past (7). However, this concept implies that trial sponsors and investigators develop comprehensive bio-specimen banks for each trial with informed consent from patients that will allow investigators to ask scientific questions before and after trials are completed to facilitate biomarker discovery and validation.
Frankly, the goals of any new cancer treatment are to allow the patient to live longer and to live better. Therefore, clinical trials in NSCLC have two important endpoints: overall survival (OS) and the QoL of that survival. All other endpoints should be considered intermediate, becoming surrogates to those important two endpoints only if formally validated. Uncertainty remains about whether an improvement in PFS represents a clinical benefit in patients with NSCLC in the same way that prolongation of survival or an improvement in symptoms and QoL does. Furthermore, to date the relationship between PFS and OS has not been established in advanced NSCLC and remains to be controversial (8).
As a primary endpoint, PFS may be acceptable in phase II trials to identify active new agents or in scenarios in which cross-over occurs and OS seen in the study population is dramatically different from that in historical controls [as was seen in the first-line EGF tyrosine kinase inhibitor (TKI) trials]. Other groups (9) have suggested that before PFS can be used as a surrogate for the OS endpoint in advanced NSCLC, it must be validated as a surrogate endpoint, and the scenarios in which the correlation applies must be determined. Until such surrogacy has been established, OS should remain the primary endpoint of clinical trials in advanced NSCLC (10).
Clinical trials in NSCLC have typically investigated agents or regimens in patients selected for study based primarily on histology, molecular biology (e.g., EGFR, ALK, c-MET, PD-1/PD-L1) and clinical characteristics. In the majority of cases this approach has resulted in only small incremental improvements in OS (Table 1) that probably reflect the impact of agents with modest efficacy in a subset of the study population that appears not to be readily identifiable. Although this work has certainly improved the lives of many patients with NSCLC, appears to be slow, costly, and empiric.

Full table
OS, defined as the time from randomization to death from any cause, is a direct measure of clinical benefit to a NSCLC patient. Patients alive or lost to follow-up are censored (19). OS offers the greatest clinical benefit, provided that QoL is not compromised. OS as an endpoint is easily measured, unambiguous, objective, and is regarded to be clinically relevant and unaffected by the timing of assessment. However, measuring OS in clinical trials requires large patient numbers and increased length of follow-up, thus potentially delaying the approval of new agents. Since the therapeutic options for patients with advanced or metastatic NSCLC are increasing, concerns that the efficacy of drugs measured by OS may be diluted in clinical trials are increasing, thereby underestimating their true clinical benefit. These concerns are based on the assumption that subsequent lines of therapy are more effective in the control arm than in the treatment arm, or that the biology of the treatment arm has changed in some way because of exposure to the study drug, making further treatments less effective—both of which are not supported by evidence (8). Furthermore, time to death remains relatively short in advanced or metastatic NSCLC (compared with time to death in breast and colorectal cancer), thus weakening the argument that OS requires prolonged follow-up for lung cancer patients. Nonetheless, with the increased success of systemic treatments, there is a need to have efficacious drugs available to patients earlier, and the search for a more accessible endpoint and a surrogate to OS is being warranted.
Food and Drug Administration (FDA) in a non-binding recommendation consider OS to be the standard clinical benefit endpoint that should be used to establish efficacy of a treatment in patients with locally advanced or metastatic NSCLC (19). The question, therefore, for OS remains: what is clinically meaningful and what are tools at hand to measure it?
Attempting to clarify these questions the American Society of Clinical Oncology (ASCO) Cancer Research Committee selected primary and secondary endpoints for potential trials that would reflect clinically meaningful benefits to NSCLC patients (20). Although PFS is a commonly used endpoint, the working group recommended to use OS as the primary measure of clinically meaningful outcome, however, it was also acknowledged that crossover in clinical trials is increasingly common, because it offers patients a greater chance to receive the experimental treatment than fixed-arm trials. In addition, it should be noted that clinical trials can be designed that demonstrate clinically meaningful outcomes even without affecting OS, such as trials that demonstrate non-inferiority compared with existing therapies with significantly less toxicity.
Patient symptoms resulting from NSCLC progression and tolerability of treatment-related toxicities are of critical importance when considering whether a new treatment produces a clinically meaningful outcome for patients (20). In general, the ASCO Committee agreed that if a therapy is less toxic than currently prevailing treatments, a smaller improvement in efficacy is acceptable. A highly toxic therapy, however, should be accompanied by an expectation of substantially greater benefit to provide a clinically meaningful outcome to patients. To address the nuances of balancing toxicity with efficacy as well as QoL outcomes, ranges of hazard ratios (HRs) and improvements of PFS and OS to describe a clinically meaningful benefit were recommended. In this regard, it was generally agreed that relative improvements in median OS of at least 20% are necessary to define a clinically meaningful improvement in outcome (20) (Table 2).
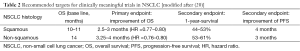
Full table
Although OS was selected as the primary endpoint by this Committee, this does not diminish the value of PFS and other surrogate endpoints as valid endpoints in certain clinical situations. This is especially true in cancer types that often produce symptoms related to progressive disease (e.g., painful bone metastases) where a significant prolongation in PFS may provide meaningful palliation and improved QoL.
The “Quality-adjusted Time Without Symptoms of Toxicity” (Q-TWiST) analysis method is frequently applied to evaluating outcomes in cancer clinical trials, but there is little information on what constitutes a clinically important difference. The overall differences between treatments for most (56%) of the observed, published values for Q-TWiST analyses are between 12% and 19% (21). Three quarters of the Q-TWiST studies had improvements in OS of 12–17%, while differences in PFS ranged from 12% to 26%. Studies that have evaluated the clinical importance of changes in QoL scores suggest that changes of 5–10% are clinically meaningful (21). Based on these findings Revicki and co-workers (21) recommended that a clinically important and meaningful difference for Q-TWiST is 10% of OS in a study, and differences of 15% are clearly clinically important. If less is known about a specific treatment and/or disease area, a clinically meaningful benefit should be greater than 5% but not more than 10% in planning sample size and statistical power (21).
Of course, trials that are designed with less ambitious goals than those described here may still be of benefit to individual patients if trial end points are met. As pointed out, there is no “single” factor which will make a trial “clinically meaningful”, but in order to establish significant advances and clinical meaningful outcomes for advanced or metastatic NSCLC patients investigators should bear in mind these challenges laid out here. These recommendations, however, are not intended to set standards for regulatory approval or insurance coverage but rather to encourage patients and investigators to demand more from clinical trials.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Ramalingam S, Belani C. Systemic chemotherapy for advanced non-small cell lung cancer: recent advances and future directions. Oncologist 2008;13 Suppl 1:5-13. [PubMed]
- Schiller JH, Harrington D, Belani CP, et al. Comparison of four chemotherapy regimens for advanced non-small cell lung cancer. N Engl J Med 2002;346:92-8. [PubMed]
- Scagliotti GV, Parikh P, von Pawel J, et al. Phase III study comparing cisplatin plus gemcitabine with cisplatin plus pemetrexed in chemotherapy-naive patients with advanced-stage non-small-cell lung cancer. J Clin Oncol 2008;26:3543-51. [PubMed]
- Paz-Ares LG, de Marinis F, Dediu M, et al. PARAMOUNT: Final overall survival results of the phase III study of maintenance pemetrexed versus placebo immediately after induction treatment with pemetrexed plus cisplatin for advanced nonsquamous non-small-cell lung cancer. J Clin Oncol 2013;31:2895-902. [PubMed]
- Sellmann L, Fenchel K, Dempke WC. Improved overall survival following tyrosine kinase inhibitor treatment in advanced or metastatic non-small-cell lung cancer-the Holy Grail in cancer treatment? Transl Lung Cancer Res 2015;4:223-7. [PubMed]
- Dempke WC, Fenchel K. Targeted therapy for NSCLC-- a double-edged sword? Anticancer Res 2015;35:2503-12. [PubMed]
- Dempke WC, Sellmann L, Fenchel K, et al. Immunotherapies for NSCLC: Are We Cutting the Gordian Helix? Anticancer Res 2015;35:5745-57. [PubMed]
- Booth CM, Eisenhauer EA. Progression-free survival: meaningful or simply measurable? J Clin Oncol 2012;30:1030-3. [PubMed]
- Buyse ME, Squifflet P, Laporte S, et al. Prediction of survival benefits from progression-free survival in patients with advanced non-small cell lung cancer: evidence from a pooled analysis of 2,838 patients randomized in 7 trials. J Clin Oncol 2008;26:abstr 8019.
- Cheema PK, Burkes EL. Overall survival should be the primary endpoint in clinical trials for advanced non-small-cell lung cancer. Curr Oncol 2013;20:e150-60. [PubMed]
- Pirker R, Pereira JR, Szczesna A, et al. Cetuximab plus chemotherapy in patients with advanced non-small-cell lung cancer (FLEX): an open-label randomised phase III trial. Lancet 2009;373:1525-31. [PubMed]
- Thatcher N, Hirsch FR, Luft AV, et al. Necitumumab plus gemcitabine and cisplatin versus gemcitabine and cisplatin alone as first-line therapy in patients with stage IV squamous non-small-cell lung cancer (SQUIRE): an open-label, randomised, controlled phase 3 trial. Lancet Oncol 2015;16:763-74. [PubMed]
- Sandler A, Gray R, Perry MC, et al. Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. N Engl J Med 2006;355:2542-50. [PubMed]
- Garon EB, Ciuleanu TE, Arrieta O, et al. Ramucirumab plus docetaxel versus placebo plus docetaxel for second-line treatment of stage IV non-small-cell lung cancer after disease progression on platinum-based therapy (REVEL): a multicentre, double-blind, randomised phase 3 trial. Lancet 2014;384:665-73. [PubMed]
- Brahmer J, Reckamp KL, Baas P, et al. Nivolumab versus Docetaxel in Advanced Squamous-Cell Non-Small-Cell Lung Cancer. N Engl J Med 2015;373:123-35. [PubMed]
- Borghaei H, Paz-Ares L, Horn L, et al. Nivolumab versus Docetaxel in Advanced Nonsquamous Non-Small-Cell Lung Cancer. N Engl J Med 2015;373:1627-39. [PubMed]
- Reck M, Kaiser R, Mellemgaard A, et al. Docetaxel plus nintedanib versus docetaxel plus placebo in patients with previously treated non-small-cell lung cancer (LUME-Lung 1): a phase 3, double-blind, randomised controlled trial. Lancet Oncol 2014;15:143-55. [PubMed]
- Yang JC, Wu YL, Schuler M, et al. Afatinib versus cisplatin-based chemotherapy for EGFR mutation-positive lung adenocarcinoma (LUX-Lung 3 and LUX-Lung 6): analysis of overall survival data from two randomised, phase 3 trials. Lancet Oncol 2015;16:141-51. [PubMed]
- FDA. Clinical Trial Endpoints for the Approval of Non-Small Cell Lung Cancer Drugs and Biologics: Guidance for Industry (published April 2015): Available online: http://www.fda.gov/downloads/drugs/guidancecomplianceregulatoryinformation/guidances/ucm259421.pdf
- Ellis LM, Bernstein DS, Voest EE, et al. American Society of Clinical Oncology Perspective: Raising the bar for clinical trials by defining clinically meaningful outcomes. J Clin Oncol 2014;32:1277-80. [PubMed]
- Revicki DA, Feeny D, Hunt TL, et al. Analyzing oncology clinical trial data using the Q-TWiST method: clinical importance and sources for health state preference data. Qual Life Res 2006;15:411-23. [PubMed]


