Editor’s note:
In the era of personalized medicine, a critical appraisal new developments and controversies are essential in order to derived tailored approaches. In addition to its educative aspect, we expect these discussions to help younger researchers to refine their own research strategies.
Pros: concurrent chemo-radiotherapy remains the ideal treatment in fit patients with large volume unresectable stage III non-small cell lung cancer
Introduction
Treatment of non-small cell lung cancer (NSCLC) remains a hotly discussed topic. In considering the wide range of disease that comprises the category of stage III NSCLC, debate about the most effective treatment grows quite intense. When we consider large volume or “bulky” disease, we typically refer to patients that are not eligible for upfront surgical resection. These patients may have large tumors in an unfavorable location (i.e., invasive or superior sulcus), large mediastinal lymph nodes, multiple involved nodal stations, or even lymph nodes with extracapsular extension. Patients suffering from disease having these characteristics are frequently recommended by national guidelines and institutional multidisciplinary tumor boards to have definitive chemo-radiotherapy (1,2). The basis of this recommendation comes from an impressive assortment of trial data conferring overall survival benefit of chemotherapy combined with radiotherapy (RT) approach, which will be described herein. Despite this data, however, there remains uncertainty of which treatment modality to use.
The combination of chemotherapy with RT (chemo-radiotherapy) can be accomplished in many ways, but is typically given sequentially or concurrently. The primary goal of this combined modality is to increase survival and local control by limiting the local disease with RT and controlling systemic spread with chemotherapy. Early approaches used induction chemotherapy prior to local (i.e., RT) treatment. In theory, this strategy may limit normal tissue toxicity by treating a reduced post-chemotherapy tumor volume. However, as one can imagine, using a “sequential” approach may lead to an increase in the overall time of treatment, which in turn may allow disease progression to go unchecked for a longer period of time. To combat potential prolonging of treatment time, investigators explored a concurrent approach of administering chemotherapy during the RT course. Concurrent therapy has been shown to be superior to sequential therapy; however, it may induce more acute toxicity (myelosuppression and esophagitis) (3). With that said, both approaches have been shown to be superior to single modality definitive RT or surgery treatment modalities. Several randomized trials comparing sequential and concurrent use of chemotherapy and RT for patients with stage III NSCLC have been reported (3-9).
Concurrent chemotherapy with RT
Definitive chemo-radiotherapy, as a treatment of choice for locally advanced disease, stems from the work of Dillman and co-workers. Their sentinel publication in 1990 of the CALGB 8433 randomized controlled trial described the definitive treatment of stage III NSCLC with a sequential approach of chemotherapy followed by RT vs. RT alone. They found a statistically significant median and overall survival improvement afforded by the sequential approach (10). This benefit was also further confirmed by RTOG 8808, which considered unresectable NSCLC treated with sequential chemotherapy followed by RT (11).
Concurrent chemo-radiotherapy as a superior treatment option, compared to sequential chemo-radiotherapy, has been shown by several phase III trials (5-8). In the West Japan Lung Cancer Study Group, Furuse et al. demonstrated an improved overall (2- and 5-year) and progression free survivals (PFS) in patients receiving concurrent cisplatin-based regimens with a split-course RT course (7). Additionally, they showed a greater disease response rate to the combined approach (7). As demonstrated by the French GLOT-GFPC NPC 95-01 data, survival can be improved in a concurrent regimen (6). The Czech study, reported by Zatloukal et al., demonstrated improved median, progression free, and overall survival in the concurrent arm (9). Curran et al. reported the findings of RTOG 9410, which further confirmed the results of chemotherapy combined with RT. This randomized trial compared the sequential “Dillman regimen” of platinum-based chemotherapy followed by a RT dose of 63 Gy to the disease vs. concurrent chemo-radiotherapy, in either a conventional or hyper-fractionated regimen. The definitive concurrent chemo-radiotherapy approach of cisplatin/etoposide with a daily RT dose of 63 Gy was found to be superior to the other arms, conferring a statistically significant median survival (MS) of 17 months and 5-year overall survival of 16% (5) (Table 1).
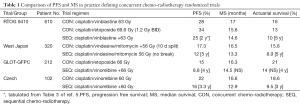
Full table
How about induction chemotherapy?
When considering if induction chemotherapy should be used, Belani and co-workers compared an induction chemotherapy strategy to a sequential and concurrent approach. They used 63 Gy for each arm and found that the concurrent CRT arm had better outcomes in regards to MS (12). Vokes et al. further reported that there was no significance difference in median or overall survival, but with upfront chemotherapy, the rate of grade 3–4 hematologic toxicity was increased (13).
Does altered RT fractionation have a role?
In effort to increase therapeutic gain, and thereby increase tumor control, investigators have considered various forms of altered fractionation (e.g., accelerated, hyperfractionated, or even hyperfractionated with concomitant boost). In this context, the United Kingdom Continuous Hyperfractionated Accelerated Radiation Therapy (CHART) and the ECOG 2597 trials were tested. These were a comparison of sequential chemo-radiotherapy with altered fractionation, concurrent treatments. In the ECOG trial, the concurrent accelerated irradiation arm had a significantly improved MS of 20.3 months compared with 14 months for patients receiving conventional daily radiation after chemotherapy (14). Similarly, the CHART trial showed a survival advantage for a continuous hyperfractionated RT regimen given 3 times a day compared to conventional, once-daily RT over a longer period (15). The unfortunate aspect of a multi-treatment per day regimen is that many patients are unable to adhere to the schedule for practical/logistical considerations, such as transportation to-and-from the treatment facility.
Dose radiation dose escalation benefit?
Some clinicians may question whether radiation dose escalation can replace chemotherapy or have a role in concurrent chemo-radiotherapy. The RTOG 93-11 dose escalation study revealed that 77.4 and 83.8 Gy are safe to administer without chemotherapy provided the V20 lung volumes are tightly respected (16). Additionally, Kong et al. have demonstrated respectable MS outcomes (19 months) in NSCLC patients receiving up to 103 Gy without chemotherapy (17). Importantly, these data remain controversial, especially in consideration of the RTOG 0617 dose escalation toxicity results (18).
Dose escalation following induction chemotherapy was attempted in the CALGB 30105 phase II trial. Its aim was to determine if dose escalation to 74 Gy in stage III a/b patients receiving concurrent chemotherapy was effective. Unfortunately, the trial closed early, however it determined that platinum-based regimens were more effective than standard thoracic RT. With that said, depending on the chemotherapy used, there was increased associated toxic with the higher dose (19).
Applying the data to patients
With this background, we can address the best utilization of definitive concurrent chemo-radiotherapy for the treatment of large volume disease from a clinical perspective. With great objectivity, we can state that there exists a NSCLC stage III patient population whereby a performance status, significant weight loss, and/or substantial co-morbidities, not only prohibits treatment by invasive surgical means, but also often precludes a concurrent chemo-radiotherapy approach. Although generally considered a suitable treatment for a mildly debilitated patient demographic, a thoughtful application of the chemotherapy and radiation must still be applied, as it should not be universally applied concurrently.
When approaching a patient with the intent to deliver concurrent chemo-radiotherapy, exclusion of surgical resection must be performed, as adjuvant chemotherapy after resection can be a very effective treatment approach. Non-resectable tumors or extensive mediastinal involvement (e.g., ≥ N2) are commonly the drive for concurrent chemo-radiotherapy. Additionally, we must consider patients that would require a surgical pneumonectomy, as candidates for concurrent chemo-radiotherapy (20). For a non-surgical candidate, but physically fit, good performance status patient, having less than 5% weight loss, we recommend concurrent chemo-radiotherapy as a standard of care. This treatment approach has many advantages, as described below.
A patient having a high performance status is more likely to complete treatment without a treatment break, whether due to insufficient blood counts, unexpected hospitalization, treatment-related fatigue or illness, or even depression. This in turn, allows for a concise treatment package time, maintenance of body weight, and the opportunity for tumor dose escalation. A patient with a good performance status can also better tolerate the anticipated toxicity of a concurrent approach, which includes increased risk of grade 3 acute esophagitis, myelosuppression, and nausea.
Ultimately, the goal of concurrent chemo-radiotherapy is to improve local control and survival. Selection of appropriate patients for this modality is paramount for successful delivery. Physically fit patients that are deemed unresectable or by personal preference are not surgical candidates benefit from this combined modality, with improved local control and PFS. Consistent with the recommendations of national organizations (e.g., ACR, NCCN, ASCO) (1,2,21), we strongly recommend concurrent chemo-radiotherapy in patients with locally advanced unresectable NSCLC.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Chang JY, Kestin LL, Barriger RB, et al. ACR Appropriateness Criteria® nonsurgical treatment for locally advanced non-small-cell lung cancer: good performance status/definitive intent. Oncology (Williston Park) 2014;28:706-10, 712, 714 passim. [PubMed]
- Ettinger DS, Wood DE, Akerley W, et al. Non-Small Cell Lung Cancer, Version 6.2015. J Natl Compr Canc Netw 2015;13:515-24. [PubMed]
- Aupérin A, Le Péchoux C, Pignon JP, et al. Concomitant radio-chemotherapy based on platin compounds in patients with locally advanced non-small cell lung cancer (NSCLC): a meta-analysis of individual data from 1764 patients. Ann Oncol 2006;17:473-83. [Crossref] [PubMed]
- Belderbos J, Uitterhoeve L, van Zandwijk N, et al. Randomised trial of sequential versus concurrent chemo-radiotherapy in patients with inoperable non-small cell lung cancer (EORTC 08972-22973). Eur J Cancer 2007;43:114-21. [Crossref] [PubMed]
- Curran WJ Jr, Paulus R, Langer CJ, et al. Sequential vs. concurrent chemoradiation for stage III non-small cell lung cancer: randomized phase III trial RTOG 9410. J Natl Cancer Inst 2011;103:1452-60. [Crossref] [PubMed]
- Fournel P, Robinet G, Thomas P, et al. Randomized phase III trial of sequential chemoradiotherapy compared with concurrent chemoradiotherapy in locally advanced non-small-cell lung cancer: Groupe Lyon-Saint-Etienne d'Oncologie Thoracique-Groupe Français de Pneumo-Cancérologie NPC 95-01 Study. J Clin Oncol 2005;23:5910-7. [Crossref] [PubMed]
- Furuse K, Fukuoka M, Kawahara M, et al. Phase III study of concurrent versus sequential thoracic radiotherapy in combination with mitomycin, vindesine, and cisplatin in unresectable stage III non-small-cell lung cancer. J Clin Oncol 1999;17:2692-9. [PubMed]
- Le Chevalier T, Arriagada R, Quoix E, et al. Radiotherapy alone versus combined chemotherapy and radiotherapy in unresectable non-small cell lung carcinoma. Lung Cancer 1994;10 Suppl 1:S239-44. [Crossref] [PubMed]
- Zatloukal P, Petruzelka L, Zemanova M, et al. Concurrent versus sequential chemoradiotherapy with cisplatin and vinorelbine in locally advanced non-small cell lung cancer: a randomized study. Lung Cancer 2004;46:87-98. [Crossref] [PubMed]
- Dillman RO, Seagren SL, Propert KJ, et al. A randomized trial of induction chemotherapy plus high-dose radiation versus radiation alone in stage III non-small-cell lung cancer. N Engl J Med 1990;323:940-5. [Crossref] [PubMed]
- Sause W, Kolesar P, Taylor S IV, et al. Final results of phase III trial in regionally advanced unresectable non-small cell lung cancer: Radiation Therapy Oncology Group, Eastern Cooperative Oncology Group, and Southwest Oncology Group. Chest 2000;117:358-64. [Crossref] [PubMed]
- Belani CP, Choy H, Bonomi P, et al. Combined chemoradiotherapy regimens of paclitaxel and carboplatin for locally advanced non-small-cell lung cancer: a randomized phase II locally advanced multi-modality protocol. J Clin Oncol 2005;23:5883-91. [Crossref] [PubMed]
- Vokes EE, Herndon JE 2nd, Kelley MJ, et al. Induction chemotherapy followed by chemoradiotherapy compared with chemoradiotherapy alone for regionally advanced unresectable stage III Non-small-cell lung cancer: Cancer and Leukemia Group B. J Clin Oncol 2007;25:1698-704. [Crossref] [PubMed]
- Belani CP, Wang W, Johnson DH, et al. Phase III study of the Eastern Cooperative Oncology Group (ECOG 2597): induction chemotherapy followed by either standard thoracic radiotherapy or hyperfractionated accelerated radiotherapy for patients with unresectable stage IIIA and B non-small-cell lung cancer. J Clin Oncol 2005;23:3760-7. [Crossref] [PubMed]
- Saunders M, Dische S, Barrett A, et al. Continuous, hyperfractionated, accelerated radiotherapy (CHART) versus conventional radiotherapy in non-small cell lung cancer: mature data from the randomised multicentre trial. CHART Steering committee. Radiother Oncol 1999;52:137-48. [Crossref] [PubMed]
- Bradley J, Graham MV, Winter K, et al. Toxicity and outcome results of RTOG 9311: a phase I-II dose-escalation study using three-dimensional conformal radiotherapy in patients with inoperable non-small-cell lung carcinoma. Int J Radiat Oncol Biol Phys 2005;61:318-28. [Crossref] [PubMed]
- Kong FM, Ten Haken RK, Schipper MJ, et al. High-dose radiation improved local tumor control and overall survival in patients with inoperable/unresectable non-small-cell lung cancer: long-term results of a radiation dose escalation study. Int J Radiat Oncol Biol Phys 2005;63:324-33. [Crossref] [PubMed]
- Bradley JD, Paulus R, Komaki R, et al. Standard-dose versus high-dose conformal radiotherapy with concurrent and consolidation carboplatin plus paclitaxel with or without cetuximab for patients with stage IIIA or IIIB non-small-cell lung cancer (RTOG 0617): a randomised, two-by-two factorial phase 3 study. Lancet Oncol 2015;16:187-99. [Crossref] [PubMed]
- Socinski MA, Blackstock AW, Bogart JA, et al. Randomized phase II trial of induction chemotherapy followed by concurrent chemotherapy and dose-escalated thoracic conformal radiotherapy (74 Gy) in stage III non-small-cell lung cancer: CALGB 30105. J Clin Oncol 2008;26:2457-63. [Crossref] [PubMed]
- Albain KS, Swann RS, Rusch VW, et al. Radiotherapy plus chemotherapy with or without surgical resection for stage III non-small-cell lung cancer: a phase III randomised controlled trial. Lancet 2009;374:379-86. [Crossref] [PubMed]
- Bezjak A, Temin S, Franklin G, et al. Definitive and Adjuvant Radiotherapy in Locally Advanced Non-Small-Cell Lung Cancer: American Society of Clinical Oncology Clinical Practice Guideline Endorsement of the American Society for Radiation Oncology Evidence-Based Clinical Practice Guideline. J Clin Oncol 2015;33:2100-5. [Crossref] [PubMed]


