The lung cancer nurse role in the management of paraneoplastic syndromes in lung cancer
Introduction
Paraneoplastic syndromes (PNS) are a group of clinical, heterogeneous disorders that are caused mainly by the production of cytokines by cancer or as an immune response to cancer rather than a direct result of the physical effects of cancer itself (1,2). The mechanisms by which PNS occur are not fully understood but are reported to occur in 10% of patients with lung cancer with the type of cancer influencing the nature of syndrome (3).
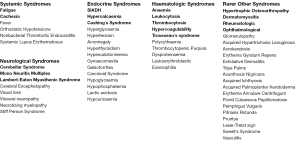
There are a wide variety of PNS that are associated with lung cancer with the most common ones being the systemic syndromes of fatigue and cachexia, paraneoplastic endocrine syndrome (PES), paraneoplastic neurological syndrome and haematological syndromes (Figure 1). Lung cancer, and in particular small cell lung cancer (SCLC), accounts for a disproportionate number and variety of PNS and these include the Syndrome of Inappropriate Anti Diuretic Hormone Secretion and Cushing’s Syndrome.
Pathways of care for patients with suspected lung cancer will usually commence with clinical evaluation, CT scan (± PET), blood screen and rapid evaluation for the next diagnostic test. PNS may be identified as part of the presenting symptom or from a blood test (such as hyponatremia or hypercalcaemia) and can help in the diagnosis of lung cancer. On rare occasions there will be a PNS syndrome present where lung cancer has not been detected despite investigations (such as a normal CT) and this is because some paraneoplastic neurological syndromes can eradicate cancer cells mediated by the immune response (4). This will always create challenges for the clinical team in determining what the actual diagnosis is and so in addition to routine tests and investigations, the testing for antibodies should be considered.
Antibodies can be detected in the serum and cerebrospinal fluid of some patients following the body’s immune response to cancer and can be helpful in diagnosing selective group of syndromes (such a paraneoplastic neurological syndrome) or types of cancer (usually SCLC). Examples of well-characterised paraneoplastic antibodies include Anti-Hu, Anti-Yo, Anti-Ri, Anti-Tr, Anti-CV2/CRMP5, Anti-Ma proteins, Anti-Amphiphysin, Anti-Recoverin, and Anti-Bipolar (2). If screening does take place for these antibodies, the results need to be treated with caution as patients without cancer can harbour paraneoplastic antibodies, variation in the consistency of the presence of antibodies can be associated with different syndromes and the absence of antibodies may not exclude a syndrome (2).
The nursing assessment
The symptoms of PNS can have a major impact on the patient’s quality of life and on individual care requirements. When symptoms of PNS occur the psychological and physical impact can be devastating to the patient and carers as immobility, discomfort, cognitive dysfunction and loss of the ability to self-care can be affected. The role of the lung cancer nurse is ideally placed to address the patient and carer concerns not only when the diagnosis is first made but throughout and beyond treatment by providing ongoing psychological support, symptom management, home care coordination and referrals to other health professionals (5,6). When the lung cancer nurse initially meets the patient it is recommended that a Health Needs Assessment is undertaken when symptoms first present, prior to starting any intervention and at the end of treatment (7). This assessment should take into account the patient’s physical, psychological, social, spiritual and practical requirements and will enable interventions to be put in place to maximise the quality of life. This assessment will provide important information for discussion at the lung cancer multidisciplinary team meeting to aid in treatment decision making. Addressing the concerns of patients and addressing their holistic needs will potentially help to improve fitness levels and potentially enhance the access to treatment (6).
Alongside the treatment plan, involvement of the palliative care services needs to be considered as it has been demonstrated that early initiation of palliative care support for lung cancer patients can improve quality of life, mood, toleration of treatment and longer survival, therefore a palliative care referral should not be delayed and limited to end-of-life care (8).
Referrals should be considered to other health care professionals including the occupational therapist and physiotherapist to maximise physical and practical capabilities. Local organisations, for example Social Services or Charities, may be able to provide help with home adaptions and to provide equipment such as wheelchairs. Additional counselling from a clinical psychologist can be considered to help with the psychological impact of the diagnosis and PNS. Family, work and finances are all likely to be affected and practical advice on how to cope and adjust should be recommended together with referral to supportive services such as complimentary therapies (massage/reflexology/YOGA) and the local lung cancer support group.
Once primary treatment, including supportive care, has been initiated, the ongoing monitoring of the patient’s condition is paramount including knowing how to contact the clinical team at any point if there are any concerns.
Treatment
Once the diagnosis of lung cancer has been established, the optimal treatment, including symptom management, for any PNS is to treat the disease and includes treatment with curative intent. There is no randomised control trial data for treatment for PNS on which to base practice but there is evidence that the anti-cancer treatments of surgery, radiotherapy, chemotherapy, biological therapies, immunotherapies, immunomodulation and immunosuppression (including glucocorticoids) may be beneficial (9). One of the challenges with PNS is that irreversible neuronal damage may have already happened by the time the diagnosis has been established and therefore whatever treatment is recommended may not necessarily help reduce the symptom burden.
There are many PNS with the most common ones now discussed together with brief description and management interventions, which should be initiated alongside the treatment of the disease. The role of the lung cancer nurse is pivotal in the management of these syndromes in liaison with the medical team.
Systemic syndromes
Fatigue
Fatigue is a highly complex syndrome, has subjective and multidimensional factors, and can be both acute and chronic. Fatigue is defined as a distressing, persistent, subjective, sense of physical, emotional, cognitive tiredness related to cancer or cancer treatment that is not proportional to recent activity and interferes with usual functioning (10). The prevalence of fatigue in cancer patients has been reported in up to 80% and up to 99% in those receiving treatment (10). Mechanisms by which cancer can cause fatigue include an increase in pro-inflammatory cytokines, dysregulation of the endocrine glands, disruption of sleep, muscle loss and cachexia (10).
Acute fatigue can be caused by factors such as infection and chronic fatigue relating more to the cancer itself or treatment. It is therefore important to assess for reversible factors including anaemia, pain, psychological distress, affected sleep, weight loss, electrolyte disturbance, medication, infection or body system abnormalities (11).
A holistic needs assessment can aid in ascertaining the potential cause of fatigue and once this has been established interventions can be identified to help ease the burden of fatigue (7). There are a number of interventions that can be recommended including:
- Advising patients to pace and plan daily activities, prioritising what is important such as food preparation and hygiene needs;
- Being physically active may also improve energy levels and increase appetite;
- Prescribing steroids in small and time limited doses, for example, dexamethasone 2 mg once a day for 2 weeks;
- Managing fatigue through anti-cancer treatments with appropriate management of side effects;
- All patients should be evaluated for the presence of fatigue after the completion of primary treatment (12);
- Fatigue caused through cachexia is discussed below.
The above advice and guidance can also help guide the patient and care givers in managing fatigue and may help to reduce the anxieties caused by the consequences of the symptoms.
Cachexia
Cachexia is defined as a multifactorial syndrome characterised by the loss of skeletal muscle mass that cannot be fully reversed by conventional nutritional support and leads to progressive functional impairment (13). The incidence of cachexia is reported in up to 60% of patients with lung cancer at the time of diagnosis (14). The symptoms of cachexia include weight loss, lack of appetite, fatigue. Cachexia is recognised as a complex metabolic disorder with the symptoms occurring not as a result of the actual cancer itself but due to the cytokines produced by the cancer. It has been demonstrated to be a poor prognostic indicator, adversely affecting performance status, increasing both comorbidities and the complications associated with treatment (15,16). The European Palliative Care Research Collaboration has developed evidence based recommendations on classification and treatment of cachexia in advanced cancer patients and states that cachexia often is overlooked, not assessed or treated adequately and is considered to be unavoidably linked with disease progression (17). As a result of this and due to the debilitating nature of cachexia, it is crucial for early and accurate assessment and appropriate interventions to be initiated (18). Initial management strategies can include:
- Assessment for potentially reversible causes such as hypercalcaemia, hyponatremia and brain metastasis;
- Utilising a local or national tool to screen for cachexia (19);
- Identifying and managing:
- Nausea;
- Sore mouth (including candida);
- Dysphagia;
- Fatigue;
- Breathlessness;
- Mouth care;
- Other symptoms;
- Prescribing food fortification or supplements;
- Giving advice on advanced food preparation;
- Prescribing medication including corticosteroids, for example dexamethasone 2 mg once a day for 2 weeks;
- Enteral feeding if appropriate;
- Referral to the dietician;
- Referral to the Speech and Language Therapist after assessment for reversible causes of dysphagia.
The lung cancer nurse assessment should include screening and monitoring for cachexia at all stages of care including psychological support to the patient and care givers (20). The above advice and guidance can also help guide the patient and care givers in managing cachexia and may help to reduce the anxieties caused by the consequences of the symptoms.
Paraneoplastic endocrine syndromes
PESs occur when a lung cancer synthesizes and secretes hormones. There are several criteria for diagnosing a PES and include an abnormal endocrine function, the absence of metastasis in an endocrine gland, deterioration of symptoms with increasing cancer burden, improvement in endocrine function with treatment and evidence of the presence of hormones in the cancer or hormone production by the cancer (3). There are a variety of PES with the most common including:
Syndrome of inappropriate antidiuretic hormone secretion (SIADH)
The diagnosis of SIADH can be confirmed by measuring serum sodium levels. This syndrome occurs due to the excessive production of antidiuretic hormone (ADH), which causes an increase in hypervolemia leading to hyponatremia where plasma sodium levels are lowered and total body fluid is increased. Approximately 10% of patients who have SCLC exhibit SIADH with symptoms including confusion, seizure, reduced consciousness and coma with these occurring due to fluid retention causing cerebral oedema (1). The treatment of SIADH includes:
- Fluid restriction to reduce the impact of fluid retention;
- Prescribing Demeclocycline which works by inhibiting ADH production;
- Prescribing Conivaptan or Tolvaptan which antagonises the effect of ADH resulting in excretion of water without electrolyte loss thereby increasing sodium levels.
Hypercalcaemia
The incidence of hypercalcaemia in patients with lung cancer is reported to be approximately 6% and is recognised as a poor prognostic indicator (21). There are two main mechanisms of action which cause hypercalcaemia. The first mechanism is where bone metastasis release cytokines, which in turn stimulate osteoclast production and action. This process accounts for approximately 20% of cases in lung cancer particularly where bone metastasis are present (22). The second most common cause is the secretion of parathyroid-related hormone. This condition is also called humoral hypercalcaemia of malignancy and is most commonly associated in squamous cell lung cancer. With both processes the diagnosis of hypercalcaemia can be confirmed by measuring serum calcium levels.
The main effects of hypercalcaemia include circulatory effects (thirst, polyuria, dehydration, renal failure), gastrointestinal effects (anorexia, nausea, vomiting, abdominal pain, constipation), neurological effects (fatigue, muscle weakness, confusion, lethargy, irritability, coma) and psychiatric manifestations (depression, anxiety, cognitive dysfunction).
The treatment of hypercalcaemia includes (23):
- The rapid intervention with ether intravenous fluids and bisphosphonates where the adjusted serum calcium is greater than 3.0 mmol/L or if there are symptoms present. Bisphosphonates work by inhibiting osteoclast bone reabsorption, which then slows bone loss. Denosumab can also be considered and is a human monoclonal antibody which works by slowing bone loss and increasing bone strength;
- Providing advice about maintaining good hydration (drinking 3–4 L of fluid per day), provided there are no contraindications (such as severe renal impairment or heart failure) where there is asymptomatic or mild hypercalcaemia (adjusted serum calcium 3.0 mmol/L or less);
- Avoiding any drugs or vitamin supplements that could exacerbate hypercalcaemia;
- Monitoring for any further symptoms of hypercalcaemia once corrected;
- Observation where anti-cancer therapy is given with monitoring and intervention as required;
- Checking serum calcium levels every three to four weeks.
Cushing’s syndrome
Cushing’s syndrome is relatively common in patients with SCLC (8–24%) and with carcinoid cancers of the lung (36–46%) with approximately 50% of Cushing Syndrome cases being neuroendocrine lung cancers (24,25). Cushing’s syndrome is caused by the excess production of adrenocorticotropic hormone (ACTH), which is triggered by the presence of cancer. This then results in increased production and release of cortisol by the adrenal glands causing symptoms of muscle weakness, weight loss, hypertension, excessive hair growth, and osteoporosis, hypokalaemia alkalosis and hyperglycaemia. The treatment of Cushing’s Syndrome includes prescribing Ketoconazole which directly inhibits cortisol secretion or Octreotide which blocks the release of ACTH.
Paraneoplastic neurological syndromes
The most common Paraneoplastic Neurological Syndromes are Cerebellar Syndrome, Mono Neuritis Multiplex and Lambert-Eaton Myasthenic Syndrome. These syndromes are not caused by the cancer itself but caused by the remote effects of the cancer when onconeural antibodies are generated in response to the development of the cancer and inadvertently attack the central and peripheral nervous system, neuromuscular junction and muscles. These syndromes are often associated with the presence of anti-Hu antibodies, which are produced together with antigen-specific T lymphocytes (26). Paraneoplastic neurological syndromes are often detected in 80% of cases before cancer is actually diagnosed with fewer than 50% have detectable antibodies (26). In patients with SCLC, up to 20% will have detectable antibodies with none of the syndromes developing. Therefore, when considering screening for antibodies, results require considered interpretation as patients without cancer can harbour paraneoplastic antibodies, variation in the consistency of the presence of antibodies can be associated with different syndromes and the absence of antibodies may not exclude a syndrome (27).
To help with the diagnosis of paraneoplastic neurological syndrome other investigations such as PET/CT may identify neurological syndrome activity, electrophysiology may confirm the syndrome (but are not always associated with cancer) and MRI can assist in the diagnosis of limbic encephalitis as atrophy can be detected.
The symptoms of Cerebellar Syndrome include gait or truncal ataxia, over or undershoot of limb movements, tremor occurring during attempted movements, impaired force and rhythm of rapidly alternating movements, ocular disturbance, head bobbing, scanning speech, rapid and slow eye movements and altered vestibular function.
The symptoms of Mono Neuritis Multiplex include painful, asymmetrical, asynchronous sensory and motor peripheral neuropathy. Multiple nerves in random areas of the body can be affected and as the condition worsens it becomes less multifocal and more symmetrical. It can be distributed bilaterally, distally, and proximally throughout the body.
Lambert-Eaton myasthenic syndrome (LEMS) is an autoimmune disease in which the body's own antibodies prevent the release of ACTH. This then interferes with transmission of nerve impulses to the muscles creating a disorder of the neuromuscular junction causing proximal muscle weakness and depressed tendon reflexes. Approximately 50% of patients have a cancer where LEMS is present. This is most common with SCLC with the incidence higher in limited rather than extensive disease (66% vs. 40%) (28).
The treatment for these syndromes include:
- Immunosuppression by utilising steroids, immunoglobulin plasma exchange or intravenous immune globulin which can all be effective in suppressing the immune response and improving the neurological symptoms;
- Considering 3,4-diaminopyridine in LEMS as this increases the release of ACTH which may ease symptoms.
Haematological syndromes
There are a number of haematological paraneoplastic syndromes that are seen in patients with lung cancer. Interventions to help ease the impact of these syndromes include primary treatment which can help to reduce the impact of each specific syndrome and often requires careful monitoring with blood screen.
The most common haematological syndrome is anaemia which contributes to fatigue and breathlessness and can be as a result of the effects of cancer on the body as well as treatment (29). Assessment of the cause of anaemia is required with appropriate interventions recommended including iron supplementation, blood transfusion or treatment modification if problematic.
Leukocytosis has a reported incidence in up to 15% of patients with non-small cell carcinoma with the cause thought to be attributed to the overproduction of granulocyte-colony stimulating factor and is associated with a poor prognosis and hypercalcaemia (21,30). Correction of hypercalcaemia, if present, is recommended together with regular monitoring of the syndrome through blood screen although this syndrome in itself rarely causes symptoms.
Thrombocytosis may be present in as many as 14% of patients with lung cancer at presentation and identified as an independent predictor of shortened survival as it is related to thromboembolic events (31). Deep Venous Thrombosis and Thromboembolism, which can cause venous thromboembolism (VTE), are the most common hypercoagulable disorders (32) with the cancer and immune system both potentially expressing procoagulant activity which ultimately cause VTE. The size, location and stage of lung cancer also contribute to the symptoms as the cancer may compress or invade large blood vessels or bulky lymphadenopathy compressing upper extremity veins leading to VTE. Other factors include increased age, obesity, inherited thrombophilia (33) as well as chemotherapy and thoracic surgery (34) which also increase the VTE risk.
Trousseau’s syndrome is a rare variant of VTE that is characterized by recurrent, migratory thrombosis in superficial veins including the chest wall and arms (35) with disseminated intravascular coagulopathy (DIC) being a disorder in which the proteins that control blood clotting become over active causing blood clots to develop (36).
With all haematological disorders careful monitoring of blood counts and clotting prior to, throughout and following intervention is crucial to prevent VTE. Close liaison with Haematologists is recommended to ensure optimal treatment.
Rarer syndromes
There are many reported additional rarer paraneoplastic syndromes, which can be seen in Figure 1. The basic premise is that primary treatment with any of the syndromes may ease the symptoms and consideration should be made in liaising with relevant specialist teams (such as Dermatology, Rheumatology, Ophthalmology) to aid in the ongoing management. Palliation of symptoms utilising analgesia, corticosteroids and other supportive interventions described earlier are also recommended.
Hypertrophic osteoarthropathy (HOA)
The diagnosis of HOA is defined by the presence of clubbing and periosteal proliferation of the tubular bones, which has been reported to be present in up to 29% of patients with non- SCLC (37). HOA is characterized by a symmetrical, painful arthropathy that usually involves the ankles, knees, wrists, and elbows. The metacarpal, metatarsal, and phalangeal bones may also be involved which can result in finger clubbing. As well as treatment of the primary cancer symptomatic interventions can also include the use of non-steroidal anti-inflammatory drugs (NSAID) and opiates with case reports showing Bisphosphonates and Octreotide being potentially effective (38).
Dermatomyositis
Dermatomyositis is a paraneoplastic syndrome characterized by inflammation of the muscles and the skin and is usually associated with adenocarcinoma of the lung. It can cause muscle weakness, has cutaneous features including necrosis, vasculitis, skin eruptions and the presence of muscle inflammation antibodies (39). Treatments, as well as primary treatment, can include the utilising of topical corticosteroids applied to affected areas on the skin and also systemic corticosteroids. Immunomodulatory medications such as Methotrexate, Mycophenolate Mofetil or intravenous immunoglobulin have been reported to be also effective (40). As sunlight can exacerbate Dermatomyositis, recommendation is made to avoid sun exposure and by applying a sunscreen including wearing photoprotective clothing.
Rheumatologic syndromes
The most frequently reported Rheumatologic Syndromes are inflammatory myopathies, seronegative rheumatoid arthritis and some atypical vasculitis with the treatment interventions focused on the management of symptoms utilising analgesics including NSAID, opiates and systemic corticosteroids (41).
Ophthalmological syndromes
Cancer associated retinopathy is probably the most common of the paraneoplastic visual syndromes and is thought to be caused by the immune response to cancer against an antigen expressed by both cancer and retina. Calcium-channel blockers and Alemtuzumab have been found to improve visual function in cancer-associated retinopathy (42). Regular Ophthalmology assessment is recommended to ensure that eyesight deterioration is minimised.
Conclusions
There are many paraneoplastic syndromes (PNS) associated with lung cancer and they can be extremely challenging to diagnose and to manage. There is no randomised control trial data to base interventions with primary treatment, symptom management, supportive and palliative care regarded as best practice. The role of the lung cancer nurse is crucial in managing the continuing care of patients and care givers with this paper aiming to guide in the understanding and describing interventions that are available for those with lung cancer PNS. Recognition by lung cancer multidisciplinary teams of PNS will help provide ongoing support to patients and consideration to their supportive care needs. Services should be responsive to patient need with close collaboration between hospital and primary care teams.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Spiro SG, Gould MK, Colice GL, et al. Initial evaluation of the patient with lung cancer: symptoms, signs, laboratory tests, and paraneoplastic syndromes: ACCP evidenced-based clinical practice guidelines (2nd edition). Chest 2007;132:149S-160S.
- Dalmau J, Rosenfeld MR. Overview of Paraneoplastic Syndromes of the Nervous System. 2014. Available online: (Accessed 17th Feb 2016).http://www.uptodate.com/contents/overview-of-paraneoplastic-syndromes-of-the-nervous-system
- Kanaji N, Watanabe N, Kita N, et al. Paraneoplastic syndromes associated with lung cancer. World J Clin Oncol 2014;5:197-223. [Crossref] [PubMed]
- Darnell RB, DeAngelis LM. Regression of small-cell lung carcinoma in patients with paraneoplastic neuronal antibodies. Lancet 1993;341:21-2. [Crossref] [PubMed]
- White J. The role of lung cancer nurse specialists. Cancer Nursing Practice 2013;12:16-22. [Crossref]
- Tod AM, Redman J, McDonnell A, et al. Lung cancer treatment rates and the role of the lung cancer nurse specialist: a qualitative study. BMJ Open 2015;5:e008587. [Crossref] [PubMed]
- National Cancer Survivorship Initiative: Holistic Needs Assessment. Department of Health 2012.
- Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 2010;363:733-42. [Crossref] [PubMed]
- Giometto B, Vitaliani R, Lindeck-Pozza E, et al. Treatment for Paraneoplastic Neuropathies. Cochrane Library 2012. Available online: . Assessed 20th February 2016.http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD007625/otherversions
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Cancer-Related Fatigue 2010; (Version 1).
- Lowe M, Molassiotis A. A longitudinal qualitative analysis of the factors that influence patient distress within the lung cancer population. Lung Cancer 2011;74:344-8. [Crossref] [PubMed]
- Bower JE, Bak K, Berger A, et al. Screening, assessment, and management of fatigue in adult survivors of cancer: an American Society of Clinical oncology clinical practice guideline adaptation. J Clin Oncol 2014;32:1840-50. [Crossref] [PubMed]
- Fearon K, Strasser F, Anker SD, et al. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol 2011;12:489-95. [Crossref] [PubMed]
- Fox KM, Brooks JM, Gandra SR, et al. Estimation of Cachexia among Cancer Patients Based on Four Definitions. J Oncol 2009;2009:693458.
- Gioulbasanis I, Georgoulias P, Vlachostergios PJ, et al. Mini Nutritional Assessment (MNA) and biochemical markers of cachexia in metastatic lung cancer patients: interrelations and associations with prognosis. Lung Cancer 2011;74:516-20. [Crossref] [PubMed]
- Laird BJ, Kaasa S, McMillan DC, et al. Prognostic factors in patients with advanced cancer: a comparison of clinicopathological factors and the development of an inflammation-based prognostic system. Clin Cancer Res 2013;19:5456-64. [Crossref] [PubMed]
- Radbruch L, Elsner F, Trottenberg P, et al. Clinical practice guidelines on cancer cachexia in advanced cancer patients. Aachen, Department of Palliative Medicinen/ European Palliative Care Research Collaborative, 2010.
- Granda-Cameron C, DeMille D, Lynch MP, et al. An interdisciplinary approach to manage cancer cachexia. Clin J Oncol Nurs 2010;14:72-80. [Crossref] [PubMed]
- Malnutrition Universal Screening Tool. Available online: http://www.bapen.org.uk/pdfs/must/must_full.pdf
- National Lung Cancer Forum for Nurses. A Practical Guide for Lung Cancer Nutritional Care 2014.
- Hiraki A, Ueoka H, Takata I, et al. Hypercalcemia-leukocytosis syndrome associated with lung cancer. Lung Cancer 2004;43:301-7. [Crossref] [PubMed]
- Horwitz MJ, Stewart A. Hypercalcemia Associated with Malignancy. In: Favus MJ. editor. Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism, 6th Edition. Washington, D.C.: American Society of Bone and Mineral Research, 2006;195.
- National Institute for Health and Clinical Excellence. Hypercalcaemia 2014; Available online: . Accessed 20th February 2016.http://cks.nice.org.uk/hypercalcaemia#!management
- Ilias I, Torpy DJ, Pacak K, et al. Cushing's syndrome due to ectopic corticotropin secretion: twenty years' experience at the National Institutes of Health. J Clin Endocrinol Metab 2005;90:4955-62. [Crossref] [PubMed]
- Shepherd FA, Laskey J, Evans WK, et al. Cushing's syndrome associated with ectopic corticotropin production and small-cell lung cancer. J Clin Oncol 1992;10:21-7. [PubMed]
- Pelosof LC, Gerber DE. Paraneoplastic syndromes: an approach to diagnosis and treatment. Mayo Clin Proc 2010;85:838-54. [Crossref] [PubMed]
- Darnell RB, Posner JB. Paraneoplastic syndromes involving the nervous system. N Engl J Med 2003;349:1543-54. [Crossref] [PubMed]
- Titulaer MJ, Wirtz PW, Willems LN, et al. Screening for small-cell lung cancer: a follow-up study of patients with Lambert-Eaton myasthenic syndrome. J Clin Oncol 2008;26:4276-81. [Crossref] [PubMed]
- Kosmidis P, Krzakowski M. Anemia profiles in patients with lung cancer: what have we learned from the European Cancer Anaemia Survey (ECAS)? Lung Cancer 2005;50:401-12. [Crossref] [PubMed]
- Kasuga I, Makino S, Kiyokawa H, et al. Tumor-related leukocytosis is linked with poor prognosis in patients with lung carcinoma. Cancer 2001;92:2399-405. [Crossref] [PubMed]
- Hamilton W, Peters TJ, Round A, et al. What are the clinical features of lung cancer before the diagnosis is made? A population based case-control study. Thorax 2005;60:1059-65. [Crossref] [PubMed]
- Bauer KA. Risk and prevention of venous thromboembolism in adults with cancer. Available online: . Accessed 4th April 2016.http://www.uptodate.com/contents/risk-and-prevention-of-venous-thromboembolism-in-adults-with-cancer?source=see_link
- Blom JW, Doggen CJ, Osanto S, et al. Malignancies, prothrombotic mutations, and the risk of venous thrombosis. JAMA 2005;293:715-22. [Crossref] [PubMed]
- De Martino RR, Goodney PP, Spangler EL, et al. Variation in thromboembolic complications among patients undergoing commonly performed cancer operations. J Vasc Surg 2012;55:1035-40.e4. [Crossref] [PubMed]
- Caine GJ, Stonelake PS, Lip GY, et al. The hypercoagulable state of malignancy: pathogenesis and current debate. Neoplasia 2002;4:465-73. [Crossref] [PubMed]
- Chattopadhyay D, Adhya S, Bandyopadhyay S, et al. Disseminated Intravascular Coagulation in Lung Cancers of Epithelial Origin. Journal of Dental and Medical Sciences 2013;9:18-22. [Crossref]
- Sridhar KS, Lobo CF, Altman RD. Digital Clubbing and Lung Cancer. Chest 1998;114:1535. [Crossref] [PubMed]
- Nguyen S, Hojjati M. Review of current therapies for secondary hypertrophic pulmonary osteoarthropathy. Clin Rheumatol 2011;30:7-13. [Crossref] [PubMed]
- Miller ML, Vleugels RA. Clinical manifestations of dermatomyositis and polymyositis in adults. Available online: . Accessed 4th April 2016.http://www.uptodate.com/contents/clinical-manifestations-of-dermatomyositis-and-polymyositis-in-adults?source=see_link
- Ang GC, Werth VP. Combination antimalarials in the treatment of cutaneous dermatomyositis: a retrospective study. Arch Dermatol 2005;141:855-9. [Crossref] [PubMed]
- Racanelli V, Prete M, Minoia C, et al. Rheumatic disorders as paraneoplastic syndromes. Autoimmun Rev 2008;7:352-8. [Crossref] [PubMed]
- Ohguro H, Nakazawa M. Pathological roles of recoverin in cancer-associated retinopathy. Adv Exp Med Biol 2002;514:109-24. [Crossref] [PubMed]


