Cytology versus histology for programmed death-ligand 1 expression evaluation in the landscape of non-small cell lung cancer patients selection for immunotherapy
Programmed death 1 (PD-1)/programmed death-ligand 1 (PD-L1) represent key targets for specific monoclonal antibody inhibitors, such as pembrolizumab, nivolumab and atezolizumab, currently used in clinical practice for the management of metastatic non-small cell lung cancer (NSCLC) patients (1). PD-L1 expression evaluation was not required to administrate nivolumab, an anti-PD-1 inhibitor, and atezolizumab, an anti-PD-L1 inhibitor, in NSCLC second-line treatment. Conversely, pembrolizumab, an anti-PD-1 inhibitor, can be administered as single-agent, only in NSCLC patients whose sample tumours show ≥50% of PD-L1 expression, in first-line (2), or ≥1%, in second-line setting (3). More recently, the KEYNOTE-189 clinical trial demonstrated that when combined with first-line chemotherapy, pembrolizumab can be administered regardless of PD-L1 expression status (4). Thus, in non-oncogene-addicted advanced NSCLC patients, especially in first-line setting, the determination of PD-L1 expression is needed despite the possibility to use the combination of chemotherapy plus pembrolizumab. The evaluation of PD-L1 expression, in absence of head-to-head trials comparing pembrolizumab versus chemotherapy plus pembrolizumab in strong-positive PD-L1 NSCLC and in order to avoid chemotherapy administration, is still of paramount importance (2). An important consideration is that the histological sample is available only in a limited number of advanced stage NSCLC patients, in relation to sample collection difficulties (2,5). This has led to the improvement of minimal invasive procedures in collecting, directly from NSCLC central or distant lesions, cytological samples both for morphological evaluation and molecular characterization. The possibility to prepare a cytology sample as a cell block to be used in the analytical procedure validated on histological samples represent an important point to properly manage NSCLC patients. To date, the evaluation of PD-L1 expression is validated using immunohistochemistry (IHC) and in all the phase III clinical trials this analysis was performed on formalin-fixed, paraffin-embedded (FFPE) tissue specimens. Based on these considerations, the reproducibility of the survival results, showed by these trials, in the clinical practice depends also on tissue samples availability.
In the Journal of the American Society of Cytopathology, Torous et al. (6) report PD-L1 expression results on 232 advanced NSCLC patient tumor specimens, 94 cytological prepared as cell block and 138 histological specimens, obtained by using the clone 22C3 pharmDx kit on the Dako Automated Link 48 platform. In particular, as reported in the study, the cytology specimens included FFPE cell blocks from EBUS-TBNA (54/94; 57.4%), pleural fluid (26/94; 27.7%), fine needle aspirates (12/94; 12.8%), and bronchial washing or brushing specimens (2/94; 2.1%). The histological specimens included core needle biopsies (83/138; 60.1%), large resections (39/138; 28.3%), and transbronchial biopsies (16/138; 11.6%).
Overall, 223/232 (96%) of analyzed specimens yielded an interpretable result. In particular, 37.5% showed a tumor proportion score (TPS) <1%, 23.7% a TPS 1–49% and 34.9% a TPS ≥50%, in line with the results obtained in the pivotal pembrolizumab clinical trials. The authors report a similar PD-L1 TPS between cytological and histological samples, with no statistically significant differences. In addition, in both cytological and histological TPS ≥50% analyzed patient cohorts, also a similar objective response (ORR) and disease control rates (DCR) to pembrolizumab were assessed. Most importantly, the reported study highlights the possibility to assess the PD-L1 expression on cytological samples prepared as FFPE cell-blocks in real life, evaluating the obtained results also in relation to pembrolizumab treatment and EGFR, ALK and ROS1 molecular evaluation (6). This point has a high clinical relevance, considering that in NSCLC patients routine setting, the more frequent (70–80%) tumor specimen available for morphological and molecular (EGFR, ALK and ROS1) evaluation may often be a cytology specimen (5).
To date, other few studies evaluated the role of cytology, in particular of cell block, as starting material for PD-L1 expression evaluation by IHC and, in general, the degree of concordance between paired cytological and histological specimens was high (7-9) (Table 1). Most of these studies were focused on paired samples (Figure 1), considering both cytology and surgical pathology specimens collected from the same patient tumor. This point is of paramount importance because, from a methodological point of view, only with paired samples a strong correlation of results may be confirmed. Conversely, in the study by Torous et al., no paired sample testing was done and the analyzed advanced stage NSCLC samples represents the real-world experience, providing a complementary evidence regarding the feasibility of PD-L1 expression evaluation on cell-block in clinical practice by using the clone 22C3 pharmDx kit (Agilent Technologies, Santa Clara, CA, USA) and its role in relation to EGFR, ALK and ROS1 evaluation (6). In fact, the assessed molecular profile was analyzed according to PD-L1 TPS and specimen types and no statistically significant differences were observed in either the overall distribution of EGFR, ALK and ROS1 alterations or the distribution of genomic alterations according to negative, low, or high PD-L1 TPS, underling the need of simultaneous testing in clinical setting to complete the panel of clinical relevant biomarkers for patients therapeutic stratification and management (10).
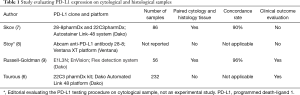
Full table

The obtained analytical data were also evaluated from the clinical point of view; in fact, on the basis of PD-L1 expression evaluation, 19 patients (11 assessed on cytology and 9 on histological samples) were enrolled and evaluated for first-line treatment with pembrolizumab. The number of patients receiving pembrolizumab therapy in this study is relatively low and the ORR and DCR were not in line with clinical trials, also if showing no statistically significant difference between the two groups of patients [ORR and DCR at 6 weeks were 20% (2/10) and 60% (6/10)respectively in the cytology cohort and 22% (2/9) and 56% (5/9) in the histological cohort]. However, some considerations should be made. The enrolled population was not homogenous. In fact, the percentage of patients with metastatic/recurrent NSCLC was between 67.7% and 73.4%. This means that about 30% of patients was affected by early stages NSCLC. This point further reduced the number of patients in which the potential role of pembrolizumab can be evaluated and consequently the weight of reported results. In addition, the outcomes reported by the authors were half of those reported by clinical trials (2). In order to clarify this issue and considering the low number of patients evaluated in this study, their clinical characteristics (i.e., performance status, tumour load, etc.) might play an important role.
Considering all together the data obtained from previous studies and the Torous et al. study (6), we can conclude that PD-L1 expression evaluation, as the current clinical approved test to select NSCLC for immune checkpoint inhibitor therapy, can be reliably assessed also on cytological samples prepared as cell block, allowing the testing of a large number of patient in relation to the data obtained from clinical trials (11). However, further studies are needed to strongly validate the cell block laboratory procedures preparation and PD-L1 data interpretation to select NSCLC patients for immunotherapy treatment in clinical practice.
Acknowledgements
None.
Footnote
Conflicts of Interest: U Malapelle—consulting or advisory role for Boehringer Ingelheim, MSD, AstraZeneca, Roche; A Iaccarino—travel grant by MSD; A Rossi—consulting or advisory role for Eli Lilly, MSD, Boehringer Ingelheim, AstraZeneca, Roche.
References
- Novello S, Barlesi F, Califano R, et al. Metastatic non-small-cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2016;27:v1-v27. [Crossref] [PubMed]
- Reck M, Rodríguez-Abreu D, Robinson AG, et al. Pembrolizumab versus Chemotherapy for PD-L1-Positive Non-Small-Cell Lung Cancer. N Engl J Med 2016;375:1823-33. [Crossref] [PubMed]
- Garon EB, Rizvi NA, Hui R, et al. Pembrolizumab for the treatment of non-small-cell lung cancer. N Engl J Med 2015;372:2018-28. [Crossref] [PubMed]
- Gandhi L, Rodríguez-Abreu D, Gadgeel S, et al. Pembrolizumab plus Chemotherapy in Metastatic Non-Small-Cell Lung Cancer. N Engl J Med 2018;378:2078-92. [Crossref] [PubMed]
- Malapelle U, Bellevicine C, De Luca C, et al. EGFR mutations detected on cytology samples by a centralized laboratory reliably predict response to gefitinib in non-small cell lung carcinoma patients. Cancer Cytopathol 2013;121:552-60. [Crossref] [PubMed]
- Torous VF, Rangachari D, Gallant BP, et al. PD-L1 testing using the clone 22C3 pharmDx kit for selection of patients with non-small cell lung cancer to receive immune checkpoint inhibitor therapy: are cytology cell blocks a viable option? J Am Soc Cytopathol 2018;7:133-41. [Crossref] [PubMed]
- Skov BG, Skov T. Paired Comparison of PD-L1 Expression on Cytologic and Histologic Specimens From Malignancies in the Lung Assessed With PD-L1 IHC 28-8pharmDx and PD-L1 IHC 22C3pharmDx. Appl Immunohistochem Mol Morphol 2017;25:453-9. [Crossref] [PubMed]
- Stoy SP, Rosen L, Mueller J, et al. Programmed death-ligand 1 testing of lung cancer cytology specimens obtained with bronchoscopy. Cancer Cytopathol 2018;126:122-8. [Crossref] [PubMed]
- Russell-Goldman E, Kravets S, Dahlberg SE, et al. Cytologic-histologic correlation of programmed death-ligand 1 immunohistochemistry in lung carcinomas. Cancer Cytopathol 2018;126:253-63. [Crossref] [PubMed]
- Malapelle U, Mayo de-Las-Casas C, Rocco D, et al. Development of a gene panel for next-generation sequencing of clinically relevant mutations in cell-free DNA from cancer patients. Br J Cancer 2017;116:802-10. [Crossref] [PubMed]
- Tsao MS, Kerr KM, Kockx M, et al. PD-L1 Immunohistochemistry Comparability Study in Real-Life Clinical Samples: Results of Blueprint Phase 2 Project. J Thorac Oncol 2018. [Epub ahead of print]. [Crossref] [PubMed]


