Coexistent pulmonary granular cell tumor and adenocarcinoma of the lung
Case report
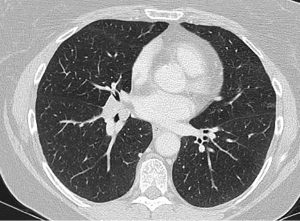
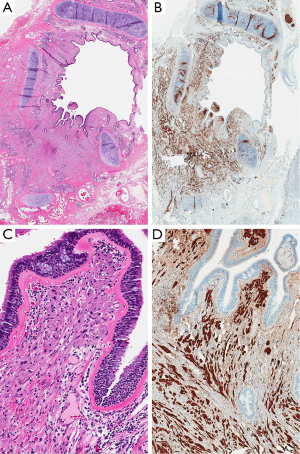
A 55-year-old Caucasian female who was a 30 pack-year smoker had a computed tomography (CT) scan of the abdomen for evaluation of abdominal pain. The CT revealed a right lower lobe (RLL) lung nodule. A CT chest confirmed the presence of a 1.3 cm × 2 cm infiltrating soft tissue mass extending into the anterior aspect of the basal medial segment of the RLL along the major fissure. In addition, there was a 5 mm right middle lobe and a 6 mm peripheral sub-pleural nodule in the RLL (Figure 1). Bronchoscopy showed an endobronchial lesion in the RLL posterior basal segment. Endobronchial biopsy showed sheets of tumor cells in the bronchial mucosa with abundant granular cytoplasm and small nuclei without significant atypia. The cells were positive for S-100 and negative for keratin AE1/AE3, synaptophysin, chromogranin and TTF-1, supporting a diagnosis of granular cell tumor (GCT). Ki-67 showed a very low proliferative index (2% of tumor cells). A staging PET/CT did not reveal any FDG-avid lesions but did show right parahilar lymphadenopathy. After multidisciplinary discussion, given the extent and infiltrative nature of her disease, surgical resection was recommended. A right thoracotomy was performed for a potential bronchoplastic procedure. With bronchoscopic guidance, the RLL was divided with a knife and frozen sections were sent of the bronchial margin. Unfortunately, this revealed GCT. A middle lobectomy was subsequently performed in order to obtain a negative margin. The resected specimen (Figure 2) revealed a 1.2 cm GCT in the RLL with morphology and immunomarkers identical to the pre-surgical biopsy, as well as a 6 mm focus of acinar-predominant adenocarcinoma in the RLL which was found by the pathologist in the subpleural parenchyma, 9 cm from the GCT. All lymph nodes were negative for malignancy. The right middle lobe also contained a 0.7 cm chondroid hamartoma and atypical adenomatous hyperplasia.
Discussion
GCT is an uncommon benign mesenchymal neoplasm that usually occurs in the upper aerodigestive tract, skin, breast or soft tissues of the extremities. The cell of origin is unknown, although neural differentiation has been suggested (1). Primary pulmonary GCTs are rare, accounting for 6-10% of all GCTs (1). The usual age at presentation is between the third and fifth decades. In a series of 19 patients with pulmonary GCT, 9 (47%) were found incidentally and 10 (53%) had obstructive symptoms (2). The lesions can be solitary or multifocal at presentation. Most cases present as an endobronchial nodule in the central airways. Although pulmonary GCT can often be successfully resected bronchoscopically, some tumors entrap submucosal glands, surround nerves and infiltrate peribronchial tissues, making bronchoscopic excision challenging. In such cases, and in tumors that are multifocal at presentation, definitive surgical resection may be warranted. Another issue impacting choice of therapy is the possibility of co-existing malignancy; six case reports and one small case series (three cases) of this occurrence have been reported (3-5). The lung cancers in these reports were of varying histologies, and it is possible that the association is coincidental. However, the existence of such cases suggests that specimens with resected GCT should be carefully examined to rule-out co-existing pulmonary carcinoma; subsequent management must be directed towards the carcinoma.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Lack EE, Worsham GF, Callihan MD, et al. Granular cell tumor: a clinicopathologic study of 110 patients. J Surg Oncol 1980;13:301-16. [PubMed]
- Deavers M, Guinee D, Koss MN, et al. Granular cell tumors of the lung. Clinicopathologic study of 20 cases. Am J Surg Pathol 1995;19:627-35. [PubMed]
- Cutlan RT, Eltorky M. Pulmonary granular cell tumor coexisting with bronchogenic carcinoma. Ann Diagn Pathol 2001;5:74-9. [PubMed]
- Gabriel JB Jr, Thomas L, Mendoza CB, et al. Granular cell tumor of the bronchus coexisting with a bronchogenic adenocarcinoma: a case report. J Surg Oncol 1983;24:103-6. [PubMed]
- Hurwitz SS, Conlan AA, Gritzman MC, et al. Coexisting granular cell myoblastoma and squamous carcinoma of the bronchus. Thorax 1982;37:392-3. [PubMed]


