
Exploring barriers to lung cancer patient access, diagnosis, referral and treatment in Kwazulu-Natal, South Africa: the health providers’ perspectives
Introduction
Every year, far too many lives across the globe are cut short by chronic diseases, such as heart disease, stroke, cancer, chronic respiratory diseases and diabetes (1). While this phenomenon was previously common in high income countries (HICs), low- and middle-income countries (LMICs) have also become the victims of chronic diseases (2). In LMICs, cancer and other non-infectious diseases, have particularly received less public attention, as a result of being historically given low priority by governments and funding agencies (3,4). However, LMICs are currently faced with a double disease burden from infectious diseases and non-communicable diseases (NCDs) (5) and this poses a unique challenge for priority setting in health systems that are already resource strapped.
The number of new cancer cases is rising almost everywhere in the world, putting an increasing strain on even the most advanced health systems (6-11). The burden of cancer has already been flagged as a serious public health problem in sub-Saharan Africa (SSA), owing to the lack of or the absence of effective cancer control programs/registries, qualified health care workers or specialists, and poor diagnostic and treatment capacity (12,13). Additionally, cancer neglect in South Africa (SA) may be attributable to being the highest HIV burdened country in the world, with the largest volume of patients on antiretroviral therapy (ART) (14-16). This, simultaneously, increased lifespan and consequent aging of the HIV positive population, resulting in an increased crude non-AIDS-defining cancer, which has been a major shift from AIDS-defining cancers to non-AIDS-defining cancers (14-16).
In SA alone, it was recently estimated that, 107,467 new cancer cases occurred, with 57,373 total deaths in 2018 (11). Breast cancer has the highest morbidity followed by cervical and prostate cancers, respectively (11). In the same period, SA’s incidence of lung cancer was reported at 7.7%, with a 4th ranking among all the cancers (11). Lung cancer had the highest mortality rate at 13.5% (11). This burden is aggravated by low suspicion index by patients and healthcare providers alike, limited financial and human resources, poorly developed healthcare systems, and limited quality care (17). Even more disheartening is the fact that overwhelming majorities of lung cancer patients are diagnosed late and the pathways of care are not clearly defined (18,19), resulting in poor health outcomes (8-10). National cancer policies identify the improvement of care coordination as a priority to improve the delivery of health services for people with cancer (20). Identification and elimination of the current barriers to effective cancer care coordination are essential for healthcare improvement purposes and would potentially increase adherence to best practices (2,6,7,21,22).
This paper describes health professionals’ views about barriers to lung cancer care, in order to use the evidence for developing intervention strategies for improving lung cancer outcomes in SA. The aim of this study was to explore the health professionals’ understanding and experiences on the barriers to lung cancer care in the three health facilities providing oncology services in KwaZulu-Natal (KZN), SA.
Methods
Study settings
This study was conducted among the oncology unit professionals from the three health facilities; namely: Greys Hospital located in Pietermaritzburg (PMB), Addington Hospital and Inkosi Albert Luthuli Central Hospital, which are both located in Durban (DBN). The health facilities were chosen on the basis that they are the only public hospitals offering oncology services in the Province. DBN and PMB, located in eThekwini and uMgungundlovu District Municipalities, respectively, are the two most populous districts in KZN Province. KZN is the second most populous province in SA, with a total population of 11.4 million people (19.7% of SA total population) (23). In 2014, the first (Gauteng) and second (KZN) most populous provinces in SA accounted for the highest number of cancer deaths, with lung cancer having the highest rates in Gauteng and second highest in KZN, respectively (24).
The public health service structure in SA and in KZN province follows a pyramidal approach, organized in referral patterns that starts from primary level through to secondary level, tertiary level, quaternary levels and medical training institutions (25). The foundation of the public health system is the primary healthcare clinics that are the first line of access for people needing healthcare services (26). Access to clinics has improved, but in many instances, the quality of health care provided at this level has weakened (26). The next tier are the district hospitals, to which patients are referred, based on the assessment of the health condition by health care professional. At the tertiary level, are the academic hospitals, where advanced diagnostic procedures and treatments are provided. The current pathway has the tendency to prolong the time for a patient to access advanced diagnostic procedures and treatment services offered at tertiary levels (25,27). Navigating through these fragmented and complex health care systems, is difficult, thereby decreasing the likelihood of favourable health outcomes and patient satisfaction (28).
Study design
This was a qualitative study, based on the grounded theory approach. The grounded theory methodology (29) is rooted in landscape interpretation and symbolic interaction, and it suggests that reality exists in the meaningful social actions of individuals, which are created through interpretational interactions. It is widely used in health and social sciences to generate theoretical accounts of social phenomena. Described as the “the most comprehensive qualitative research methodology available” (30), this approach is appropriate when research aims to explain a process where the concerns of those involved are central to its understanding and cannot be predetermined (29,31). The study used in-depth interviews, which allowed probing and posing of follow-up questions to generate rich data. Interviews were conducted using general interview guide approach, due to its flexibility to allow the reordering of questions during the interview process (32). Interviews were audio-recorded (with participants’ permission) and each lasted approximately 35–45 minutes. Observational data was recorded daily as field notes and triangulated with data from interviews and review of relevant documents. They were transcribed by a professional transcriber, de-identified and checked for accuracy by the lead author.
Study population
The targeted potential participants were mainly the healthcare providers with extensive experience in lung cancer patient care, across a variety of geographic and health care settings and disciplines in the three public oncology facilities in KZN. Potential participants were approached by the lead investigator and only consenting eligible participants were enrolled in the study.
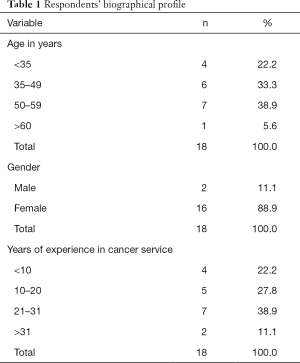
Recruitment procedures
Selection of the participants was initiated using purposive sampling and after the seventh interview, we continued through theoretical sampling, in order to complete the categories and concepts created from previous interviews, until saturation was achieved. Purposive sampling was used to recruit the participants who had different specialties and involvement in the provision of oncology services, experiences (33) and the study objectives. The main goal was to focus on particular characteristics of the health professionals that are of interest, which would best enable the researcher to answer the research questions. Over time, to meet the needs of theoretical sampling and reach saturation, diversity was sought in work experience, age, facilities, and number of years specializing in oncology. Eighteen health care professionals participated in the study, with theoretical saturation reached at 19 in-depth interviews, whereby no new issues emerged (34). The sample included oncologists with various specialties (n=7), radiotherapists (n=4), pulmonologist (n=1), social workers (n=2), a psychologist (n=1) and nurses (n=3). Participant demographics are presented in Table 1.
Full table
Data collection
In line with the criteria followed in planning in-depth interviews (32) these steps were followed:
- Step 1: identified and listed healthcare providers who were considered information-rich and willing to participate in our study.
- Step 2: developed all instruments for the interviews to be conducted. An interview protocol was developed, which covered how and where to start each interview, how and when to end or conclude it, how the data was to be correctly and ethically recorded and what will be done after the interview.
- Step 3: an interview guide was then developed with questions and issues to be explored, probes and informed consent forms. The issues in the interview guide were grouped by their thematic areas.
- Step 4: a research training was scheduled for the data collectors, interview guides with a clear purpose were set up and the consent forms.
- Step 5: summaries of key findings from the collected data were made immediately after each interview, thereby identifying areas for further probing in subsequent interviews.
Through the courtesy of hospital management, the interviews were conducted in the uninterrupted office space within the three health facilities. All participants signed informed consent forms prior to their participation. The interview guide consisted of five main parts. The first part focusing on awareness and accessing healthcare for lung cancer. The second and third parts were meant to get an understanding of the barriers to patient care and management for lung cancer in KZN. The fourth part was focused more on the priority areas for improving lung cancer management, and lastly, the fifth were for respondents’ demographics.
Data analysis
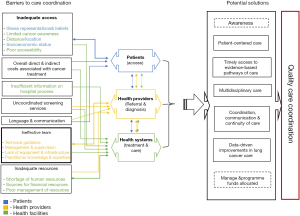
Data collection and analysis took place concurrently, allowing each proceeding interview to be informed by those which preceded it. The analysis was achieved through the use of transcripts complemented with handwritten field notes. The interviews were transcribed verbatim to ensure that the transcripts represented the information contained in audio files. Thematic analysis was used to analyse the data. This is one of the most common forms of analysis in qualitative research, capable of emphasizing, pinpointing, examining, and recording themes within data (35). Our approach to the analysis was hybrid, informed by a conceptual framework (Figure 1), the study objectives and new themes emerging from the data. NVIVO version 12 software was used to facilitate the analysis.
For reporting of the qualitative study findings, four supporting processes of trustworthiness were applied, namely conformability, dependability, credibility and transferability. Credibility was confirmed by selecting the appropriate data collection tools. This was informed by a presentation of the tools to the Multinational Lung Cancer Control Program (MLCCP) team, a bigger project that the current study is part of. The researchers interviewed participants for their views and experiences in their practice environment. Furthermore, member check was used to prolong the involvement of the researcher to increase the credibility of the data. Dependability was established by detailed data analysis and direct references to the professional experiences of the respondent. The conformability and consistency of the analysis were maintained through analyst triangulation, as means to assure rigor in the analysis process, where transcripts were shared with all authors and later emerging themes were discussed and agreed upon.
Ethical consideration
The study obtained the ethics approval and gatekeeper permission from the University of KZN Biomedical Research Ethics Committee (Ref: BE332/18) and KZN Provincial Department of Health (HRKM Ref: 007/18 and NHRD Ref: KZ_201801_031). All the three participating health facilities supported the study. Selected healthcare providers voluntarily signed informed consent forms prior to participating in the study. Confidentiality was maintained through anonymizing their contributions in all written materials.
Results
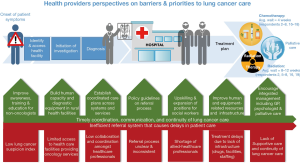
In the following sections the presentation of results is divided in four main thematic areas of care continuum, namely; (I) access, (II) referral, (III) diagnosis, and (IV) treatment and care, under which key themes are based. The first theme describes the barriers to accessing care and contains two subthemes: “Low lung cancer suspicion index” and “Distance to health facilities”. The remaining three themes relate to the barriers to care presenting at or within the health services context. The referral theme includes one subtheme: “Inadequate communication between healthcare professionals”. Diagnosis includes two subthemes: “Late diagnosis” and “Collaboration and coordination amongst healthcare professionals” and finally, the last theme included two sub-themes: “Inadequate resources”, “Supportive care and continuity of lung cancer care” and “Shortage of allied-healthcare professionals”. The participants consisted of 2 males and 16 females, with the ages and years of experience in cancer service ranging from 31 to 74 and 8 to 50, respectively (Table 1).
Access
Timely access to primary healthcare and well-coordinated transition from primary care through to tertiary care services are key pillars to patient care. Two sub-themes emerged as paramount to patient access, and these are low lung cancer suspicion index and distance to health facilities.
Low lung cancer suspicion index
There is a co-existing malignancy, so that is the first thing, lack of knowledge on the part of the health care worker, not necessarily a doctor, but maybe a primary care worker. Professionals at these lower level facilities are not sufficiently equipped and trained, resulting in substandard performance in early diagnosis and referral. At the symptom onset point, misclassification of lung cancer as tuberculosis (TB) affects patient access to lung cancer care (respondents 2, 3, 5–8, 10–12, 15, 16), with the following comment from an oncology nurse:
“Physical barriers would be a lack of resources or lack of knowledge in the periphery. So, they might present with a chronic cough or deliberate breathing to maybe a primary health facility, where there is no doctor to assess, and might be tested for TB or started on TB medication. TB might be co-existing with a malignancy, and because it is so prevalent in our settings, they might just be worked out for TB, treated for TB and go back home.. As a result of the large number of patients in our health facilities, there are waiting times to get into those initial district hospitals before they can be referred on to regional.” (respondent 7)
Limited lung cancer knowledge appeared to affect patient access both at health provider and patient level. If any of the two or both lacked knowledge on lung cancer, patient access is affected. “I think firstly, there is poor insight, a lot of people don’t know what cancer really is and how severe it can be and because of that they often leave it to the point where it’s quite debilitating before they attend to it”, a pulmonologist mentioned. There was convergence of views among the healthcare providers in articulating a need to go to illiterate rural dwellers, with services and awareness campaigns, in order to improve the patient access to cancer care (respondents 2, 3, 5–8, 10–12, 15–18). The department needs to somehow spare an effort to educating peripheral hospitals, the government needs to provide educational services at clinics, as echoed by an oncology nurse. However, two participants dismissed any suggestion that there is limited lung cancer knowledge, especially in rural areas (respondents 4, 13). One radiotherapist gave the following comment on this:
“I think our patients know about lung cancer, but for many of them, it is difficult to distinguish its symptoms. Same as for some healthcare providers, but we are seeing a lot of awareness happening… Another issue maybe is that, although most of them have already heard the word ‘umdlavuza’ (cancer) and they have some concept of it, they do not exactly know what it entails. I think that is dependent very much on the patient’s social circumstances, educational background, cultural understanding of what cancer is, and I think that is very variable, it depends who your patient is and where they (are) coming from.” (respondent 4)
Another point raised was that community members are only informed about cancer issues when it is cancer month, with no post-cancer awareness follow-up, yet TB receives priority focus (respondents 3, 6, 11). One radiotherapist claimed, “They are not well informed, information is not good enough to be cascaded to the people. Only when it is cancer month, we see and hear about awareness and after that there’s nothing. Priority is in TB.” (respondent 6)
Distance to health facilities
Concerns were expressed regarding the burden of travel from a patient’s residence to healthcare providers. The necessity for repeated visits for lung cancer diagnosis and treatment on an outpatient or an inpatient basis, thereby making distance an issue with which the patient must manage during the disease course (respondents 1–3, 5–8, 10–12, 16–18). Rurality impacts on access to proper diagnostic and treatment services; the more remote people are, the harder it is for them to access adequate health services, especially since, in KZN, oncology services are located within the major cities of DBN and PMB. Referring to this, an oncologist said:
“The third thing that distresses me is how challenging daily living is for our patients; getting to tertiary hospitals might take two days… I am amazed at their patience and their fortitude, I think somebody like me would just give up… They come a day before to line up in the cold outside some hospital waiting for transport to leave at 05:00 o’clock to come here, and you have got cancer, and you are nauseous, and you can’t sit properly in the long bumpy bus ride. That is horrific and the journey back and the hours spent waiting to see the doctor here, so if you think too much about that, then you realize how difficult it is for our patients actually to get here.” (respondent 17)
Referral
Inadequate communication between healthcare professionals
The inconsistent, delayed and incomplete communication amongst the health care team, whereby patients often find themselves lost in a disjointed medical care system, emerged as the most important barrier to effective referral system (respondents 1–3, 7, 8, 15, 16, 18). It was evident that organized resources are unavailable to health providers of people with advanced lung cancer or any other cancer for that matter. There were also strong sentiments suggesting that health providers in the primary healthcare facilities misdiagnosed patients (respondents 1, 2, 5–10, 15–19).
“It (referral procedures) works at the moment, but it could be a lot better because we (experienced oncologist), find that patients are not often worked up appropriately. Not everybody gets referred to a pulmonologist, they might be referred directly to us and they don’t come with all necessary investigations, histological and blood work. Reasons being, the base hospitals themselves, their facilities are so overburdened. Patients don’t get called back for blood results, so we often faced with having to search and look for things or re-book patients for CT scans, and that delays us in terms of our decision making.” said an oncologist (respondent 5).
Referral patterns can drastically impact on the ability of individual patient to obtain high quality treatment. The delay in time between identifying a need for a specific test or treatment and actually receiving those services can negatively impact health and costs of care (respondents 3, 5–9, 11, 15, 16, 18, 19). These results highlight a persistent need to develop and evaluate interventions to improve the provision of information between primary and specialist care, because information exchange is not timely and effective (respondents 2, 5–9, 11, 12, 15–17).
Diagnosis
Late diagnosis
Late presentation of patients is a challenge, and most of them come with outstanding investigations, thereby delaying the diagnosis process (respondents 1, 4–7, 9, 13–17). In addition, a majority are from rural areas, where health-seeking behavior remains relatively poor (respondents 1, 4–7, 9, 11, 13–17, 19). Lung cancer cases at the time of detection is, on average, markedly advanced. Other health care settings issues included lack of care coordination, and of effective screening tools for early detection of lung cancer. Following that, was the issue of timeliness. This is the health care system’s ability to provide health care quickly after a need is recognized and make appropriate and necessary referrals (respondents 2–7, 8–11, 16). Inadequate knowledge and expertise of practitioners in public primary healthcare clinics, again, proved to be one of the major sources of the diagnosis barrier, resulting in late presentation (respondents 2, 3, 5–8, 10–12, 15–16). Attesting to this assertion, one of the nurses stated:
“What I found in many cases whether it’s lung, or especially lung actually, that patients have symptoms and going to the clinic and reporting the symptoms has not helped. In the meantime, this disease is going on so I think that it’s all good and well for patient to start off at the primary health clinic, but I think more skills are needed there to identify problems because majority of my patients tell me it’s been going on for such a long time and then finally now they have found out what it is.” (respondent 3)
Collaboration and coordination amongst healthcare providers
There was a firm view advocating for a better and proactive coordination amongst different sectors, settings and professionals (respondents 5–9, 11–13, 17, 19). A point was made that the introduction of clear referral pathways, guidelines, joint protocols or service agreements between these healthcare settings may help address these issues (respondents 6, 9, 15). Additionally, because most people have easy access to primary healthcare facilities, nurses and doctors within those facilities should be trained on lung cancer or cancer in general, including the screening protocols (respondents 4, 9, 15, 18, 19). In explaining the health systems structure in SA, one oncologist participating in this study stated:
“You know the South African health care system, it starts at the primary health clinic and then the district hospitals and then the general hospitals and then regional hospitals and then finally they come to the tertiary health facilities. An unfortunate issue is that the only diagnosis services that are functional in KZN are in large tertiary hospitals… There needs to be a fast track for suspected lung cancer to go to a dedicated clinic, dedicated CT scan, dedicated pulmonology to look at those patients quickly.” (respondent 15)
Treatment and care
Inadequate resources
All participants identified an under-supply of various health care professionals throughout the public sector of SA, particularly oncology specialists (respondents 1–19). The current staff shortage was raised as a barrier to effective care coordination that could adversely affect patients’ care across their entire cancer care continuum. This shortage places a burden on existing specialists who have to manage large patient volumes, with inadequate resources (respondents 1–19). Moreover, for some provinces, if not all in SA, public sector does not have targeted treatment (respondents 2, 5–8, 16, 19). One chemo nurse and an oncologist shared, respectively:
“We cater for a lot of patients but are understaffed and less equipped and therefore treatment gets booked very late even after the patients have accessed the facilities.” (respondent 12)
“Our lifetime of the equipment is 12 years and it has reached that, and we get faults now and again but fortunately we are able to fix them. That poses a delay, because it will probably be down for plus/minus 2 weeks, of which everything comes to a halt. For that time, it becomes a chaos, because now patients that were on treatment, will not continue with treatment over 2 weeks. We need a very highly sophisticated software system that can organize that for us, but obviously we cannot see that happening very soon. So, we just have to deal with what we have and of course, some patients that fall through the gaps.” (respondent 17)
Supportive care and continuity of lung cancer care
The lack of communication and effective referral between the health facilities emerged an important issue affecting the patient treatment and care (respondents 1–3, 7–13). These are particularly evident through the tertiary institutions’ inability to refer patients received from the tertiary institutions back to the local facilities, where patients sought support services. It emerged that patients often don’t get referred back into local support services they need when they have sought treatment elsewhere and it is then left to the patient to present themselves to local hospitals for the continuity of care and support (respondents 1–3, 5, 7–13, 16). There is a need for a care plan across services and across facilities or settings. A radiation-oncology therapist and a medical officer gave the following comments on this:
“We have long delays in our radiotherapy treatment times, so from the time they get into the clinic to the time they get treated with radiotherapy is up 6 to 9 months and one of the reasons is because we have a lack of larger facilities for these patients, our machine, which is only one machine, that’s an old machine that can only treat so many patients within a day, we have a lack of radiotherapy staff to deliver or carry out the treatment that is prescribed.” (responded 13)
“Human resource is a very big factor, you have a limited number of specialists as well. People go to private practice because sometimes you feel demotivated when you are working in a place where you cannot access what you want, you cannot give the patient best treatment you could if you were in a different setting. It makes you feel like you have failed patients and having to tell the patient now and again, I can’t do this because I am limited.” (respondent 8)
Shortage of allied-healthcare professionals
Related to supportive care services noted above, a number of healthcare providers noted that socio-economic hardship ran the spectrum from everyday financial concerns. Issues such as providing for one’s family while undergoing treatments; needing additional support to be able to cope with the disease; and requiring finances to travel to receive treatments (respondents 1–3, 5, 7–13, 16). One social worker remarked:
“Each area requires a dedicated social worker and we are unable to provide that dedication because there are only 6 of us in the hospital and we are carrying maybe about 8 to 12 units per social worker, so it does become difficult to provide the dedicated services needed to lung cancer patients, in the case.” (respondent 2)
A psychologist also added that, when you receive a diagnosis of cancer, and you don’t have anywhere to vent about it, or none to experience it with, and it makes it more difficult to manage the disease. Participants described a range of examples that included loss of bodily functions as a result of the treatment or lung cancer (respondents 1–11, 13–19). It is suggested that, these could cause anxiety and depression (respondents 3, 5–9). A radiation oncologist stated:
“Even for the patient, accepting that I have a problem, accepting that I can’t breathe, I can’t walk here to my car on a daily basis when I used to do that and be independent and losing my independence, every one of them needs to be seen. It’s not about seeing them once and doing a grant, there is so much more that needs to be done, the support, the counselling, just lending that helping hand to them, because now sweetie we are just touching the surface.” (respondent 11)
Inadequate resources and a lack of integrated psychosocial care were identified as barriers to comprehensive cancer care (respondents 1–9, 11–15, 19). The need for social workers and psychologists was identified as an urgent workforce priority. In addition, the health professionals agreed that KZN hospitals lacked specialist palliative care physicians and services (respondents 1–19).
The findings presented in this paper can be summarized through the following illustrative diagram (Figure 2). The bottom part of the illustration presents key barriers to lung cancer patient care, whereas the green middle layer shares potential solutions to the barriers presented. The upper part presents the pathway through which lung cancer patients can receive care. The illustrated key findings of current barriers and solutions has the potential to guide the development of future initiatives to achieve coordinated quality lung cancer care. It is important to note that the referral systems barrier cuts across all points of the continuum, as well as those highlighted in the figure. Therefore, addressing the inefficient referral systems would result in timely coordination, communication and continuity of lung cancer care in SA, as indicated below.
Discussion
In this study the high burden of disease was attributed to, among other barriers, limited access to oncology services, as well as poor diagnostic and support services. This could be due to factors, such as, socio-economic status, under-resourced facilities, resulting in weak or ineffective healthcare systems, poor accessibility to health care services, lack of inter-sectoral alliance, and shortage of health care professionals adding to the lack of intra-sectoral collaboration. The study further found that lung cancer is usually diagnosed late when the disease is at an advanced stage, thereby making treatment, where available, largely ineffective. Even then, there is another waiting period for treatment to be initiated, because of the lack of human or equipment-related resources.
One of the greatest barriers to accessing lung cancer care in SA is the lack of geographic access to healthcare facilities and lack of well-trained primary care providers, which result in poor distribution of services across the country (37). There were strong sentiments from this study supporting that the location of large specialist centers in urban areas primarily present physical and economic challenges to patients residing in remote rural areas, including distance, limited access to transport and the cost of travel. The health care context was described as contributing to delays, and themes included lack of multidisciplinary management, where referral procedures as a barrier extended across the care continuum. Barriers such as excessive waiting times may affect care-seekers who have low incomes and live in neighborhoods of social and economic distress. It is left to the public health system to provide good health for the greatest number of people by locating essential health services and personnel within communities, where they are most accessible to the largest number of people.
Our results revealed that the current pathways are more of a barrier than an enabler, thus resulting in poor health outcomes. In considering the challenges of access, such as lack of geographic access (37), psychosocial barriers and weak health systems (38,39), focusing on upskilling and expansion of multidisciplinary positions may contribute to improving lung cancer care. Multidisciplinary positions worth considering include social workers, psychologists, palliative carers and other primary healthcare workers, as most patients in SA are entering the health system at the primary care level (26). Additionally, as patients obtain more information, their decision-making capacity increases and their response to the disease improves, thereby enhancing their quality of treatment and care (40). Some studies, including a systematic review (41), have demonstrated that there is a need for supportive care among patients with lung cancer.
There is adequate literature supporting the need for, and benefit of, care coordination for people affected by cancer (6,20,27,42-52). The main challenges of the public healthcare sector in SA have been related to the burden of disease and the country’s inability to effectively plan for meeting health needs in the country (26), with competing health priorities. The right of access to health care services requires the provision of equal and timely access to basic preventative, curative, rehabilitative health services and health education; regular screening programs and appropriate treatment, preferably at community level (26). Indeed, studies in several countries have reported that more remote patients were less likely to be diagnosed before they died (20). Based on our findings, it can be argued that, where few or no services exist, the emphasis should be on establishing a core of expertise and limited cancer management, with a potential for scale-up.
In addition to the above-mentioned supportive care barriers, healthcare professionals in KZN also perceived access and diagnosis as the top barriers to effective lung cancer care. These barriers therefore call for a speedy action to lessen the grave threat that lung cancer inflicts to the health of South Africans (24). The inadequacy of systems that support access to healthcare services gives aid to the rising numbers of lung cancer fatalities in SA (11,24). The identification of current obstacles has the potential to guide the development of future initiatives to achieve coordinated quality lung cancer care. Policy-makers, administrators, and providers should incorporate the vital contributions of social work professionals in policies and programs supporting cancer care. As cancer prevention and treatment initiatives continue to develop, there is a need to support palliative care services, as they offer a realist approach to equitable, accessible and cost-effective intervention. The solutions suggested by this study cut across the South African health systems, as far as cancer is concern, and have informed the MLCCP project, with a centre of excellency for lung cancer and mobile screening being established.
The most important strength of this study was its ability to capture and analyze the perspectives of different types of healthcare practitioners/specialists working in the public healthcare facilities, providing oncology services in KZN-SA. As a limitation, it was focused on oncology healthcare providers within tertiary level hospitals, negating the contribution of primary health care facilities in cancer patient care. There is a need to explore lower level healthcare facilities which are readily available for patients, especially in the rural areas, since they compound the barriers to lung cancer care. Despite these constraints, the study produced invaluable insights into the issues affecting lung cancer patient care. Furthermore, in our knowledge this is the first study in SA that assessed the perspectives of all key types of healthcare practitioners working in the public healthcare facilities, providing oncology services in KZN-SA. Such information is lacking in the scientific body of knowledge.
Conclusions
In conclusion, our study found that limited access to oncology services and poor diagnosis to be the leading barriers to effective lung cancer care. The gross insufficiency of trained health workers adversely affects what can be achieved, especially in rural settings (26). Delays at different levels of care continuum, namely: access, diagnosis, and treatment, have serious ramifications to achieving quality care for lung cancer patients (20). Development and evaluation of interventions based on these findings is now required to improve the quality of cancer care. Furthermore, the study has provided essential information that inform policy development and planning of prevention strategies in supporting and improving cancer care in SA. National policies should (I) prioritise the provision of psychosocial support to lung cancer patients; (II) ensure adequate treatment supply, distribution and prescription; (III) educate health care workers and the public to increase awareness, knowledge and skills; and (IV) implement palliative care services in all levels of society with support from communities. Recognizing the burden of lung cancer and the forthcoming strain this imposes on health infrastructure and resource allocation in SA, begs a multipronged interventional approach to tackling this issue.
Acknowledgments
The authors would like to thank the University of KwaZulu-Natal for the provision of resources towards this study. This study forms the basis of a master’s in medical science research report. I would like to express my sincere appreciation to the Multinational Lung Cancer Control Program (MLCCP) team for their support and encouragement throughout the process.
Funding: This work was supported by Bristol-Myers Squibb Foundation (grant number 1011).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study obtained the ethics approval and gatekeeper permission from the University of KwaZulu-Natal Biomedical Research Ethics Committee (Ref: BE332/18) and KwaZulu-Natal Provincial Department of Health (HRKM Ref: 007/18 and NHRD Ref: KZ_201801_031). All the three participating health facilities supported the study. Selected healthcare providers voluntarily signed informed consent forms prior to participating in the study. Confidentiality was maintained through anonymizing their contributions in all written materials.
References
- Schmidt H. Chronic Disease Prevention and Health Promotion. In: Barrett DH, Ortmann LH, Dawson A, et al. editors. Public Health Ethics: Cases Spanning the Globe. Springer, 2016.
- Dunn J, Garvey G, Valery PC, et al. Barriers to lung cancer care: health professionals' perspectives. Support Care Cancer 2017;25:497-504. [Crossref] [PubMed]
- Institute of Medicine Committee. The National Academies Collection. In: Sloan FA, Gelband H. editors. Cancer Control Opportunities in Low- and Middle-Income Countries. Reports funded by National Institutes of Health. Washington (DC): National Academies Press (US) National Academy of Sciences, 2007.
- Urman A, Josyula S, Rosenberg A, et al. Burden of Lung Cancer and Associated Risk Factors in Africa by Region. J Pulm Respir Med 2016;6:340. [Crossref]
- Beaglehole R, Bonita R, Horton R, et al. Priority actions for the non-communicable disease crisis. Lancet 2011;377:1438-47. [Crossref] [PubMed]
- International Agency for Research on Cancer. World cancer report 2008. Lyon, France: IARC, 2008.
- World Health Organisation. Cancer. Geneva: WHO Media Centre, 2018 September 12. Available online: http://www.who.int/mediacentre/factsheets/fs297/en/
- World Health Organisation. The global burden of disease. Geneva, 2004.
- World Health Organisation. Cancer del. Geneva, 2019. Available online: http://www.who.int/cancer/en/
- World Health Organisation. Cancer. Geneva, 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/cancer
- World Health Organisation. South Africa. Globocan 2018.
- Islami F, Torre LA, Jemal A. Global trends of lung cancer mortality and smoking prevalence. Transl Lung Cancer Res 2015;4:327-38. [PubMed]
- Schluger NW, Koppaka R. Lung disease in a global context. A call for public health action. Ann Am Thorac Soc 2014.407-16. [Crossref] [PubMed]
- Antiretroviral Therapy Cohort Collaboration. Causes of death in HIV-1-infected patients treated with antiretroviral therapy, 1996-2006: collaborative analysis of 13 HIV cohort studies. Clin Infect Dis 2010;50:1387-96. [Crossref] [PubMed]
- Crum-Cianflone N, Hullsiek KH, Marconi V, et al. Trends in the incidence of cancers among HIV-infected persons and the impact of antiretroviral therapy: a 20-year cohort study. AIDS (London, England) 2009;23:41-50. [Crossref] [PubMed]
- Shiels MS, Pfeiffer RM, Gail MH, et al. Cancer burden in the HIV-infected population in the United States. J Natl Cancer Inst 2011;103:753-62. [Crossref] [PubMed]
- National Academies of Sciences Engineering and Medicine. 2 The Diagnostic Process. Improving Diagnosis in Health Care. Washington, DC: The National Academies Press, 2015:36.
- Carter-Harris L, Hermann CP, Draucker CB. Pathways to a lung cancer diagnosis. J Am Assoc Nurse Pract 2015;27:576-83. [PubMed]
- Evans WK, Ung YC, Assouad N, et al. Improving the quality of lung cancer care in Ontario: the lung cancer disease pathway initiative. J Thorac Oncol 2013;8:876-82. [Crossref] [PubMed]
- Walsh J, Harrison JD, Young JM, et al. What are the current barriers to effective cancer care coordination? A qualitative study. BMC Health Serv Res 2010;10:132. [Crossref] [PubMed]
- Balogh EP, Ganz PA, Murphy SB, et al. Patient-centered cancer treatment planning: improving the quality of oncology care. Summary of an Institute of Medicine workshop. Oncologist 2011;16:1800-5. [Crossref] [PubMed]
- Chatwin J, Sanders C. The influence of social factors on help-seeking for people with lung cancer. Eur J Cancer Care (Engl) 2013;22:709-13. [Crossref] [PubMed]
- Mid-year population estimates. South Africa: Statistics South Africa, 17 July 2018.
- Made F, Wilson K, Jina R, et al. Distribution of cancer mortality rates by province in South Africa. Cancer Epidemiol 2017;51:56-61. [Crossref] [PubMed]
- Kutzin J, Barnum H. How health insurance affects the delivery of health care in developing countries," Policy Research Working Paper Series 852, The World Bank. Available online: https://ideas.repec.org/p/wbk/wbrwps/852.html
- Jobson M. Structure of the health system in South Africa. South Africa: Khulumani Support Group, 2015.
- Gaafar R. SC17.05 Lung Cancer in Africa: Challenges and Perspectives. J Thorac Oncol 2017;12:S115-6. [Crossref]
- Meade CD, Wells KJ, Arevalo M, et al. Lay navigator model for impacting cancer health disparities. J Cancer Educ 2014;29:449-57. [Crossref] [PubMed]
- Corbin J, Strauss A. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. 3rd edition. Los Angeles: SAGE, 2008.
- Haig BD. Grounded theory as scientific method. The Philosophy of Education’s 1995 Yearbook. Champaign, IL: Philosophy of Education Society, 1995.
- Lingard L, Albert M, Levinson W. Grounded theory, mixed methods, and action research. BMJ 2008;337:a567. [Crossref] [PubMed]
- Boyce C, Neale P. Conducting in-depth interviews: A Guide for Designing and Conducting In-Depth Interviews for Evaluation Input. Monitoring and Evaluation – 2. Watertown, USA: Pathfinder International, 2006.
- Setia MS. Methodology Series Module 5: Sampling Strategies. Indian J Dermatol 2016;61:505-9. [Crossref] [PubMed]
- Dworkin SL. Sample Size Policy for Qualitative Studies Using In-Depth Interviews. Arch Sex Behav 2012;41:1319-20. [Crossref] [PubMed]
- Guest G, MacQueen KM, Namey EE. Applied Thematic Analysis. SAGE 2012.
- Australia C. Lung Cancer Framework: Principles for Best Practice Lung Cancer Care in Australia. Australia: Australian Government, 2018.
- Tegegne TK, Chojenta C, Loxton D, et al. The impact of geographic access on institutional delivery care use in low and middle-income countries: Systematic review and meta-analysis. PLoS One 2018;13:e0203130. [Crossref] [PubMed]
- Pesec M, Sherertz T. Global health from a cancer care perspective. Future Oncol 2015;11:2235-45. [Crossref] [PubMed]
- Tetteh DA, Faulkner SL. Sociocultural factors and breast cancer in sub-Saharan Africa: implications for diagnosis and management. Womens Health (Lond) 2016;12:147-56. [Crossref] [PubMed]
- Krishnasamy M, Wilkie E, Haviland J. Lung cancer health care needs assessment: patients' and informal carers' responses to a national mail questionnaire survey. Palliat Med 2001;15:213-27. [Crossref] [PubMed]
- Maguire R, Papadopoulou C, Kotronoulas G, et al. A systematic review of supportive care needs of people living with lung cancer. Eur J Oncol Nurs 2013;17:449-64. [Crossref] [PubMed]
- Aberg L, Albrecht B, Rudolph T. How health systems can improve value in cancer care. Health International, 2012.
- Bradshaw D, Groenewald P, Laubscher R, et al. Initial burden of disease estimates for South Africa, 2000. S Afr Med J 2003;93:682-8. [PubMed]
- Busolo DS, Woodgate RL. Cancer prevention in Africa: a review of the literature. Glob Health Promot 2015;22:31-9. [Crossref] [PubMed]
- Cancer Plan for the African Continent 2013-2017. Adewole IF, Denny L, Odedina F, et al. editors. African Organisation For Research & Training in Cancer, 2013:1-88.
- Carrillo JE, Carrillo VA, Perez HR, et al. Defining and targeting health care access barriers. J Health Care Poor Underserved 2011;22:562-75. [Crossref] [PubMed]
- ACE Lung Cancer Pathway Cluster. Lung Cancer Pathways: Interim Report. Variations in performance and practice. 2016. Available online: https://www.cancerresearchuk.org/sites/default/files/lung_interim_report.pdf
- Efstathiou N, Ameen J, Coll AM. Healthcare providers' priorities for cancer care: A Delphi study in Greece. Eur J Oncol Nurs 2007;11:141-50. [Crossref] [PubMed]
- Jacobsen MM, Silverstein SC, Quinn M, et al. Timeliness of access to lung cancer diagnosis and treatment: A scoping literature review. Lung Cancer 2017;112:156-64. [Crossref] [PubMed]
- Morhason-Bello IO, Odedina F, Rebbeck TR, et al. Challenges and opportunities in cancer control in Africa: a perspective from the African Organisation for Research and Training in Cancer. Lancet Oncol 2013;14:e142-51. [Crossref] [PubMed]
- Olesen F, Hansen RP, Vedsted P. Delay in diagnosis: the experience in Denmark. Br J Cancer 2009;101:S5-8. [Crossref] [PubMed]
- World Health Organization. Guide to cancer-early diagnosis. Geneva, 2017. Report No. 924151194X.


