
Preoperative and postoperative radiotherapy (RT) for non-small cell lung cancer: still an open question
Introduction
Adjuvant postoperative radiotherapy (PORT) or preoperative radiotherapy (preRT) has been advocated for decades, but despite testing and evaluation through many trials and meta-analyses a clear-cut answer concerning its use remains elusive. This is largely due to the limitations of the randomized trials, current developments in diagnostic procedures (e.g., PET-CT), the techniques of surgery and RT [from 2D to 3D-CRT and intensity-modulated radiotherapy (IMRT) with image-guided RT], and the use of pre- or postoperative chemotherapy for stage II or III disease. Hence, the current question is how to combine RT with chemotherapy or—shortly—with immunotherapy for stage III non-small cell lung cancer (NSCLC). Indeed, based on several trials and meta-analyses, chemotherapy as an adjuvant or induction treatment has become the standard practice (1,2). Furthermore, stage III patients not amenable for surgery are not treated by exclusive RT but with the addition of chemotherapy either in a sequential or concurrent manner. Concurrent chemoradiotherapy (CRT) has been shown to provide longer survival through better local control than a sequential approach (3). In the present review, we summarize the more recent publications with consideration to past publications and meta-analyses, consider if these new findings may modify our approach, and discuss how we can adapt our current practice.
preRT
The ultimate goal of preRT is to improve patient survival through better local control. One of the main advantages of this approach is its direct action on the tumor, allowing for downstaging, complete resection of tumors initially considered inoperable, or even a pathologic complete response. PreRT also allows for the control of microscopic disease. The downsides of preRT, however, are the current limitation to define the precise tumor extent even with our modern imaging techniques. By postponing of surgery by a few weeks, there is a risk of induced severe toxicity or tumor progression in case of no response or during the interval between the end of the induction treatment and surgery (4). There is also an increased risk of postoperative complications.
Preoperative, compared to postoperative RT, has been less scrutinized by randomized trials, and the available data refer mainly to CRT approaches. Many phase II trials have reported a higher response rate, more downstaging, and more pathologic complete responses, but also more postoperative complications for CRT compared to chemotherapy alone (5,6). Induction chemotherapy has often been advocated for stage III disease, but the superiority of triple-modality approach is debatable. Indeed, in trials investigating various preoperative strategies, the pathologic complete response rate with CRT ranged between 18% and 33%, compared to 10–19% with induction chemotherapy (ICT) alone (1,7,8). In a phase III trial conducted in Germany, more than 500 patients with stage IIIA or IIIB NSCLC were randomized between ICT followed by surgery and PORT, or ICT followed by an accelerated course of preoperative CRT preCRT (9). The number of complete resections was similar in both arms (84 patients in the ICT arm and 98 in the preCRT arm), but still less than 60% of the randomized patients underwent surgery. Complete pathological response with ICT and preCRT was achieved in 17 and 59 patients, respectively, but this difference did not translate into a survival benefit: 5-year survival rates were around 15% for both arms. This trial was actually not a comparison between preCRT and induction chemotherapy, but rather an evaluation of preRT vs. PORT, as the patients in the induction chemotherapy arm also received PORT. In a recent analysis from the US National Cancer Database, among 1,936 patients with T1–T2N2 disease treated with either preCRT or ICT, the pathologic complete response was higher after preCRT compared to ICT (14.2% vs. 4%), but at the expense of increased perioperative mortality and with no improvement in overall survival (10). In a retrospective study based on data from the Surveillance Epidemiology and End Results (SEER) database, the propensity score matching-based analysis showed that, compared to surgery alone, preRT increased cancer-specific survival (HR: 1.427, P=0.014) and overall survival (HR: 1.220, P=0.002) (11). One of the most important biases and limitations of this retrospective database analysis was whether chemotherapy was used concurrently with preRT.
Three randomized trials were specifically designed to compare ICT and preCRT in patients presenting with N2 disease that was initially considered resectable. In the Swiss trial, 232 patients were randomized between ICT followed by surgery 4 weeks later, or ICT followed by RT (44 Gy in 22 fractions and 3 weeks) and surgery 3 to 4 weeks later (12). This trial found no difference between the arms in terms of progression-free survival and overall survival. A R0 resection was performed in 91% and 81% of patients who did and did not undergo RT, respectively. A pathologic complete response was achieved in 16% and 12% of patients, respectively. Of note, no operative mortality was reported after RT. The sequential approach used in this study is questionable with consideration to the superiority of a concurrent approach in patients administered definitive CRT. Additionally, 15 patients in each arm did not receive the treatment according to the randomization, getting either RT in the chemotherapy-only arm, or no RT in the combined modality arm. A meta-analysis including the three available trials did not identify any benefit in terms of survival, likely due to the small number of patients (56 and 46, respectively) in the two other trials (13,14). The pooled results demonstrated that compared to ICT alone, preCRT was more effective in terms of tumor response, mediastinal downstaging, and pathological complete response of mediastinal lymph nodes. In addition, increase in perioperative mortality in the CRT group, and a higher number of patients from this group underwent a R0 resection. A similar conclusion was seen in the analysis of the US National Cancer Database which included around 2,000 patients with T1–T2N2 disease (10).
Many preRT trials used doses around 45 Gy in 5 weeks, or a biologically equivalent dose. Higher radiation doses have been advocated in small series to achieve a higher response rate, but one concern is the possible acute and long-term toxicity. Small series have showed the feasibility and safety of operation after higher RT doses, even those above 60 Gy, by taking specific measures during surgery and during the recovery period. Using the National Cancer Database, Sher at al. found a better survival of preoperative RT (preopRT) doses between 45 and 54 Gy; increasing RT doses lee to more complete pathological response without an increase in surgical morbidity or lethality (15). However, this study had all the limitations related to using a too-large database. In another small series of 52 patients, 18 were treated with doses of 60 Gy or higher. The pathologic complete response was higher compared to lower doses but no difference was observed in survival at the price of an increase in long-term noncancer mortality (16). Recently, our Spanish colleagues reported on 99 patients treated either with preopCRT or ICT. After CRT, pathologic complete response and nodal down staging were significantly higher, while loco-regional recurrence was significantly lower, but this did not translate in any survival benefit (17). Pathological response after ICT or preopCRT has been reported from different series with a wide range of values, and patient selection and the definition of a pathologic complete response vary from study to study (Table 1). Clearly, prospective studies are needed to determine these unresolved issues.
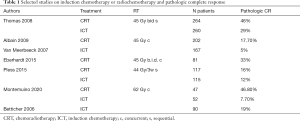
Full table
One concern related to ICT is a risk of delay between its termination and the initiation of local treatment wherein an accelerated repopulation of cancer cells and tumor regrowth can occur (4). This is even truer when the decision on the use of surgery is taken only after the induction treatment. Accordingly, there is no direct correlation between the radiologic and pathologic tumor response after induction CRT (18). In the case of no resection or incomplete resection, the chances for the patient to have an optimal curative treatment are jeopardized, as the preRT dose is too low to achieve an effective local control. Moreover, the addition of a boost delivered after several weeks of RT interruption is not very effective due to tumor repopulation.
Superior sulcus tumor
PreCRT is a commonly used strategy in patients with superior sulcus tumors. Two phase II trials conducted in the US and Japan (including 110 and 76 patients, respectively) used a concurrent approach including 45 Gy RT combined with cisplatin/etoposide or cisplatin/vindesine/mitomycin chemotherapy. Patients with N2 disease were excluded from these trials. The 5-year survival rates were 44% and 56%, respectively (18,19). Important prognostic factors were R0 resection and pathologic complete response. Of note, in the US trial, 32 out of 110 patients were not eligible for surgery. Another approach shown to be feasible is the delivery of full dose preRT (66 Gy in fractions of 2.75 Gy) concurrently with daily cisplatin (20). In a series of 115 patients observed between 1994 and 2006, 49 patients were treated with CRT either before surgery (19 patients including 2 cases of N2 disease) or as a definitive treatment (30 patients). The 5-year survival rates were 33% after trimodality therapy and 18% after CRT alone (20). Importantly however, the patients subjected to the trimodality approach were highly selected. In a recent series of Robinson et al. (21) including 107 consecutive patients treated between 1994 and 2016, 53 patients were administered with preCRT, 34 with ICT followed by PORT, and 15 with primary surgery followed by adjuvant therapy. The 5-year survival in the entire group was 45%, with no difference between the induction regimens (47% each), and 36% in the non-induction group. CRT led to a higher complete pathologic response rate (38% vs. 3%) but at the expense of higher postoperative toxicity. Strict interpretation of this study is hampered by patient selection and differences in general management over a period of 22 years. In NSCLC, the hospital volume and patient selection (T3 vs. T4, N0 vs. N1–N2) play a major role. Performing a well-designed trial study comparing induction CRT vs. ICT is challenging due the rare occurrence of superior sulcus tumour.
Postoperative radiotherapy (PORT)
The goal of PORT is to control any possible microscopic disease left after surgery at the level of the bronchial stump, or in the hilar and/or mediastinal nodes in order to increase local control and survival. Apparent benefits of PORT have been demonstrated for rectal, breast, and head and neck cancers. PORT for lung cancer may, however, induce severe toxicities to vital organs including the lungs, spinal cord, and heart.
PORT after a complete resection (R0)
One meta-analysis published in 1998, and updated in 2005 and in 2016, included the individual data of patients from 9, and later 11 trials (22-24). The initial analysis showed a paradoxically deleterious effect of PORT in pathological stage I–III NSCLC, with an absolute detriment of 7% at 2 and 5 years after a complete resection. While this negative effect was mainly observed for pathological stage I and II, no definitive conclusion could be made for stage III. Both updated analyses confirmed the harmful effect of PORT (23,24). This negative result led to a change in clinical practice, with fewer patients treated with PORT even for N2 disease. However, interpretation of available data is difficult, as many analyzed trials have been conducted over four decades. These early trials used obsolete radiation techniques such as 2D RT, posterior spinal block, cobalt-60 machines, single-plane dosimetry, or no image guidance. A new meta-analysis stratifying the PORT trials by the use of a cobalt-60 unit vs. linear accelerators showed an increased overall survival and better local control in stage III disease for trials using a linear accelerator (25). Furthermore, the irradiated volume included the whole mediastinum from the sternal notch to the lower mediastinum leading to a high heart dose. A comparison of radiation plans used in the studies included in the meta-analysis versus current techniques revealed a poor target coverage and excessive toxicity in the older techniques (26). For example, with these techniques the target coverage reached only 65%. The percentage of heart volume receiving at least 30 Gy (V30) was 35% compared to 16% with modern techniques, and the lung V20 was 25% vs. 18%, respectively. Clearly, there are no indications for PORT after a complete resection of a N0 disease, and this is in good agreement with the pattern of failure, as the locoregional relapse rate in N0 is below 5% but may be as high as 47% for N2 disease (27).
Since 1998, many papers, including single-center experiences, database analyses, and meta-analyses of randomized or non-randomized trials, have been published with conflicting results. In a recent publication based on the SEER database, PORT provided an overall survival benefit only in a subgroup with a high lymph node ratio (the ratio of the number of positive nodes to the number of examined nodes) (28). A meta-analysis based on 1 randomized trial and 12 retrospective studies also showed a benefit in pN2 disease with more than 3 positive lymph nodes (29). The LungArt trial (NCT00410683) has been designed to assess the possible benefit of PORT after a complete resection of pN2 NSCLC, with disease-free survival as the primary endpoint (30). Patients may have had ICT or postoperative chemotherapy before being randomized. The study is now closed after recruiting the required number of patients, and results are expected shortly.
Currently, adjuvant chemotherapy is recommended after a complete resection for stage II and III NSCLC (2). The question is not only the value of PORT, but also its efficacy and optimal combinations with chemotherapy. In an old randomized trial including 488 patients with pN2 disease randomized between RT (50.4 Gy) alone or in combination with four cycles of cisplatin and etoposide, no difference was found in the pattern of failure and survival (31). In contrast, in the ANITA trial investigating the role of adjuvant chemotherapy with cisplatin and vinorelbine, centers had to declare upfront whether or not they used PORT (32). Out of the 224 randomized patients, 116 received PORT, and the 5-year survival in this subset was 47%, compared to 34% for the adjuvant chemotherapy-alone subset and 17% for the no-adjuvant-treatment subset. The sequence of adjuvant chemotherapy and RT has not been tested in a randomized clinical trial, but some data are available from retrospective analyses. Based on the US National Cancer Database series, a comparison was made between concurrent postoperative CRT and a sequential approach (mostly chemotherapy followed by PORT) in 1924 pN2 patients who underwent a complete resection between 2004 and 2014 (33). The median survival for the sequential and concurrent approaches was 53 months and 37 months, respectively, and the difference was maintained in a propensity matching analysis. While the precise reasons for this difference are unknown, these might have included more toxicities or more advanced cases in the concurrent approach. In another series that specifically included ypNO or N1 disease, the 5-year loco-regional failure rate was 31% and constituted the first site of failure in 51% of patients. The figures were significantly higher for pN1 vs. pN0 disease.
Another relevant issue is the role of PORT after ICT for N2 disease, since local relapse in this subset is around 30% as the first site of relapse (25,34,35). Whereas persistent N2 disease after ICT is an evident adverse prognostic factor, the role of PORT in subjects with and without pathologic complete response, along with the role of additional chemotherapy and its optimal combination with PORT (sequentially vs. concurrently) remains unclear. In a series of 501 patients with cN2 disease treated with ICT, 99 had residual ypN2 disease, 69 of whom (70%) received PORT (36). An isolated local recurrence occurred in only 3 patients (with no impact of PORT), and distant failure occurred in 57 patients. In another series, 150 patients with pN2 disease were treated with ICT: 86 had either persistent N2 or an incomplete resection, and PORT was delivered to 70 patients. The cumulative incidence of local relapse was not very different between PORT and no PORT (47% vs. 49.5%). The PORT group included patients with more positive margins or persistent N2 (37). Surprisingly, there were more cardiac events in the no-PORT group.
The role of PORT in the case of chest wall invasion in which an R0 resection is clearly the most important prognostic factor, also remains uncertain (38). There are no data to support PORT in this subset, but retrospective studies suggest a benefit of adjuvant chemotherapy. In a study of the US National Cancer Database that included 2,326 patients, adjuvant chemotherapy was associated with a significantly better median survival (71 vs. 39 months, P<0.001), and this difference remained significant in a matched pair analysis (39).
One group with a relatively high risk of local relapse are patients undergoing sublobar resection. One of the approaches for this group is postoperative brachytherapy. In a phase III trial, 224 patients with tumors up to 3 cm in size were randomized to receive a perioperative suture containing 125I seeds parallel to the resection margins, or surgery alone (40). The dosimetry goal was to deliver 100 Gy at 5–7 mm along the central axis of the resection margin. Local progression occurred in only 17 patients, with no impact of brachytherapy even in patients with potentially compromised margins.
Incomplete resection and PORT
Another issue with no clear consensus is the role of PORT in patients with incomplete resection (R1, R2). The European Society of Medical Oncology (ESMO) conducted a survey asking 768 medical oncologists and radiation oncologists from 41 European countries about their approaches in this group of patients (41). PORT was proposed by 48% of participants, and the recommended doses ranged from 54 to 60 Gy. This fact is well illustrated in the US National Cancer Database analysis which included 3,461 patients with R1 or R2 resection treated between 2004 and 2011: 41% had no postoperative treatment, 13% had PORT, 15% had adjuvant chemotherapy, and 28% had CRT (42). The use of PORT yielded no survival benefit as opposed to adjuvant chemotherapy, irrespective of additional RT. Available data are from registries or institutional experiences with often conflicting results. In the large series based on the US National Cancer Database, incomplete resection including R1 was found to be an independent factor of poor prognosis for all stages (43). Outcomes seem to be better for patients with R1 resection at the level of the bronchial tree (44). In the series including 72 patients, PORT with doses above 54 Gy led to improved local control, but local progression still remained the major pattern of failure (45). In our own experience, in 82 patients administered PORT (50–60 Gy) after an incomplete resection, the 5-year survival rate was 27% after R1 and only 6% after R2 resection (personal unpublished data). In the US National Cancer Database analysis, of the 3,395 patients with an incomplete resection (1,892 R1 and 129 R2), 1,207 were administered PORT and about 50% of the entire group also received adjuvant chemotherapy (46). Both PORT and chemotherapy were associated with improved survival. This benefit was more pronounced for N0 disease, with a 5-year survival of 41% vs. 26% for the groups with and without PORT, respectively. An interesting observation was the impact of the radiation dose: doses between 50 and 70 Gy were associated with an improved survival, while this was not the case for higher doses. Using the same database, in a cohort of 1,446 patients with an incomplete resection (R1 or R2), only a trend was observed in favor of sequential vs. concomitant chemoradiation (median survival of 36.3 vs. 30.5 months) (47). However, this study should be interpreted with caution due to known limitations and the biases of all registries.
In situ carcinoma at the bronchial resection margin is another issue. In a large review from the literature, the presence of in situ carcinoma at the margin did not carry adverse prognosis, with the 5-year survival ranging from 50% to 100% in cases of pN0 disease, even without any adjuvant treatment (48).
According to the International Association for the Study of Lung Cancer, the definition of incomplete resection includes a nodal capsular rupture. Limited data are available for this phenomenon, as it has been rarely analyzed separately in published series. Its negative impact has been reported in the literature review by Vansteenkiste et al. (49). In our retrospective analysis of 83 patients with bulky pN2, the use of PORT was associated with a statistically significant higher OS rate in patients with extracapsular nodal extension but not in those without it (HR =0.518; 95% CI, 0.276–0.971; P=0.040 and HR =2.052; 95% CI, 0.495–8.507; P=0.322, respectively) (50). Although the sample size was limited, this unexpected finding may indicate that extracapsular nodal extension in the mediastinum is an early sign of clinically occult distant metastases in bulky pN2 patients, and that the benefit of PORT in these patients is confined to better local control. The NCCN guidelines recommend adjuvant CRT (either sequential or concurrent) for R1 resection and the latter approach for R2. For stage II, an alternative for R1 is a re-excision, and CRT for R2 (51).
PORT toxicity
One of the major concerns regarding PORT is the risk of toxic effects, particularly in the lungs and heart. PORT is considered a hazardous approach, especially after a pneumonectomy, when maximal sparing of the remaining lung is indispensable to avoid life-threatening toxicities, as seen in even the earliest studies. Another issue is the dose to the heart. The analysis of patients’ data from the SEER treated before and after 1988 showed that cardiac toxicity related to PORT was observed in the earlier, but not in the later cohorts (52). A Polish study evaluating the cardio-respiratory functions in patients who did and did not receive modern-technique PORT demonstrated no increased non-cancer radiation-induced mortality or deterioration of lung functions (53). The meta-analysis of the oldest trials on using linear accelerators showed that the evolution from conventional 2D to 3D-CRT has clearly alleviated radiation toxicity (25). However, it is unclear whether more sophisticated modern techniques, such as IMRT, can further improve the toxicity profile. A comparison of dosimetric plans using 3DCRT, IMRT, and volumetric modulated arc therapy RT in 10 patients administered PORT for pN2 disease failed to single out a technique with absolute dosimetry advantages for all patients (54). Therefore, the selection of technique should be based on each individual case using the best compromise between target coverage (efficacy) and the protection of the organs at risk. The use of protons may be another step towards reducing RT-induced toxicity.
Target volume (TV) delineation
Another issue related to PORT is the TV delineation. In preparation of the LungArt trial, two cases (one after lobectomy and one after pneumonectomy) were subjected to a dummy run procedure (55). Seventeen expert radiation oncologists were asked to define their clinical tumor volume (CTV) and planning (PTV). Huge interclinician delineation variations were observed, with PTV ranging from 148 to 1,342 cc after lobectomy, and from 187 to 1,262 cc after pneumonectomy. These variations could largely be reduced by using guidelines for TV definition. As uniformity and quality assurance of TV have a clear impact on outcome, the LungArt trial requested each center to present cases to make sure that there were no violations of the protocol guidelines.
Several studies have investigated the pattern of regional failure according to the tumor location. In the study of Feng et al. (56), failures of right-sided tumors included mainly unilateral hilar, subcarinal, and right lateral nodes, whereas failures from left-sided tumors occurred in 4R, 7, 4L, 6, 10L and 5 nodal stations; i.e. on both sides of the mediastinum. Likewise, in the study of Billiet et al. (37) which included patients with N2 disease treated by ICT followed by surgery, most loco-regional relapses occurred in the lymph node stations involved at diagnosis, with mainly a unilateral pattern for right-sided tumors, and bilateral relapses for left-sided tumors. Kępka et al. (57) used a CTV limited to the bronchial stump, the positive lymph node stations. and the uninvolved lymph node stations with high probability of microscopic disease such as the ipsilateral hilum or the subcarinal nodes. They observed an 11% local recurrence rate within a limited CTV, and only 2% outside the CTV. According to the European SocieTy for Radiotherapy & Oncology (ESTRO) and the Advisory Committee in Radiation Oncology Practice (ACROP) guidelines, CTV includes resected involved anatomical mediastinal lymph node regions, the bronchial stump, the ipsilateral hilum, and nodal stations 4 and 7. PORT should also follow other ACROP recommendations regarding contouring, planning, and treatment delivery (58). In case of preRT, the CTV is usually limited to the known tumor volume and the positive lymph node stations.
Conclusions
The role of RT adjunctive to surgery, both administered pre-and postoperatively, remains unclear, especially for pN2 NSCLC. Data indicate a better locoregional control with postoperative RT and a better tumor response with preoperative chemoradiotherapy compared to ICT, but this does not necessarily translate into survival benefit. This inconsistency is likely related to the pattern of failure after surgery for NSCLC, with a prevailing role of distant metastases, and due to multiple competing risks accompanying this malignancy. Future research should be focused on identifying patient subgroups with increased risk of local failure and on the role of combined approaches including immunotherapy.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Jacek Jassem and Rafal Dziadziuszko) for the series “Radiotherapy in thoracic malignancies” published in Translational Lung Cancer Research. The article was sent for external peer review organized by the Guest Editors and the editorial office.
Peer Review File: Available at http://dx.doi.org/10.21037/tlcr-20-472
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tlcr-20-472). The series “Radiotherapy in thoracic malignancies” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- NSCLC Meta-analysis Collaborative Group. Preoperative chemotherapy for non-small-cell lung cancer: a systematic review and meta-analysis of individual participant data. Lancet 2014;383:1561-71. [Crossref] [PubMed]
- NSCLC Meta-analyses Collaborative Group. Adjuvant chemotherapy, with or without postoperative radiotherapy, in operable non-small-cell lung cancer: two meta-analyses of individual patient data. Lancet 2010;375:1267-77. [Crossref] [PubMed]
- Aupérin A, Le Péchoux C, Rolland E, et al. Meta-analysis of concomitant versus sequential radiochemotherapy in locally advanced non-small-cell lung cancer. J Clin Oncol 2010;28:2181-90. [Crossref] [PubMed]
- Chen CP, Weinberg VK, Jahan TM, et al. Implications of delayed initiation of radiotherapy: accelerated repopulation after induction chemotherapy for stage III non-small cell lung cancer. J Thorac Oncol 2011;6:1857-64. [Crossref] [PubMed]
- Stupp R, Mayer M, Kann N, et al. Neoadjuvant chemotherapy and radiotherapy followed by surgery in selected patients with stage IIB non-small-cell lung cancer: a multicentre phase II trial. Lancet Oncol 2009;10:785-93. [Crossref] [PubMed]
- Kim HK, Cho JH, Choi YS, et al. Outcomes of neoadjuvant concurrent chemoradiotherapy followed by surgery for non-small-cell lung cancer with N2 disease. Lung Cancer 2016;96:56-62. [Crossref] [PubMed]
- Albain KS, Swann RS, Rusch VW, et al. Radiotherapy plus chemotherapy with or without surgical resection for stage III non-small-cell lung cancer: a phase III randomised controlled trial. Lancet 2009;374:379-86. [Crossref] [PubMed]
- Eberhardt WE, Pöttgen C, Gauler TC, et al. Phase III Study of Surgery Versus Definitive Concurrent Chemoradiotherapy Boost in Patients With Resectable Stage IIIA(N2) and Selected IIIB Non-Small-Cell Lung Cancer After Induction Chemotherapy and Concurrent Chemoradiotherapy (ESPATUE). J Clin Oncol 2015;33:4194-201. [Crossref] [PubMed]
- Thomas M, Rübe C, Hoffinecht P, et al. Effect of preoperative chemoradiation in addition to preoperative chemotherapy: a randomised trial in stage III non-small-cell lung cancer. Lancet Oncol 2008;9:636-48. [Crossref] [PubMed]
- Krantz SB, Mitzman B, Lutfi W, et al. Neoadjuvant chemoradiation shows no survival advantage to chemotherapy alone in Stage IIIA Patients. Ann Thorac Surg 2018;105:1008-16. [Crossref] [PubMed]
- Chen D, Wang H, Song X, et al. Preoperative radiation may improve the outcomes of resectable IIIA/N2 non-small-cell lung cancer patients: A propensity score matching-based analysis from surveillance, epidemiology, and end results database. Cancer Med 2018;7:4354-60. [Crossref] [PubMed]
- Pless M, Stupp R, Ris HB, et al. Induction chemoradiation in stage IIIA/N2 non-small-cell lung cancer: a phase 3 randomised trial. Lancet 2015;386:1049-56. [Crossref] [PubMed]
- Katakami N, Tada H, Mitsudomi T, et al. A phase 3 study of induction treatment with concurrent chemoradiotherapy versus chemotherapy before surgery in patients with pathologically confirmed N2 stage IIIa nonsmall cell lung cancer (WJTOG99303). Cancer 2012;118:6126-35. [Crossref] [PubMed]
- Chen Y, Peng X, Zhou Y, et al. Comparing the benefits of chemoradiotherapy for resectable stage III A/N2 non-small cell lung cancer: a meta-analysis. World J Surg Oncol 2018;16:8-10. [Crossref] [PubMed]
- Sher DJ, Fidler MJ, Seder CW, et al. Relationship between radiation therapy dose and outcome in patients treated with neoadjuvant chemoradiation therapy and surgery for stage IIIA non-small cell lung cancer: a population based, comparative effectiveness analysis. Int J Radiat Oncol Biol Phys 2015;92:307-16. [Crossref] [PubMed]
- Bharadwaj SC, Vallières E, Wilshire CL, et al. Higher versus standard preoperative radiation in the trimodality treatment of stage IIIa lung cancer. Ann Thorac Surg 2015;100:207-13. [Crossref] [PubMed]
- Montemuiño S, Dios NR, Martín M, et al. High-dose neoadjuvant chemoradiotherapy versus chemotherapy alone followed by surgery in potentially-resectable stage IIIA-N2 NSCLC. A multi-institutional retrospective study by the Oncologic Group for the Study of Lung Cancer (Spanish Radiation Oncology Society). Rep Pract Oncol Radiother 2020;25:447-55. [Crossref] [PubMed]
- Rusch VW, Giroux DJ, Kraut MJ, et al. Induction chemoradiation and surgical resection for superior sulcus non-small-lung carcinomas: long-term results of Southwest Oncology Group Trial 9416 (Intergroup Trial 0160). J Clin Oncol 2007;25:313-8. [Crossref] [PubMed]
- Kunitoh H, Kato H, Tsuboi M, et al. Phase II trial of preoperative chemoradiotherapy followed by surgical resection in patients with superior sulcus non-small-cell lung cancer: report of Japan Clinical Oncology Group trial 9806. J Clin Oncol 2008;26:644-9. [Crossref] [PubMed]
- Kappers I, Klomp H, Koolen MG, et al. Concurrent high-dose radiotherapy with low-dose chemotherapy in patients with non-small cell lung cancer of the superior sulcus. Radiother Oncol 2011;101:278-83. [Crossref] [PubMed]
- Robinson LA, Tanveytyanon T, Grubbs D, et al. Induction chemoradiotherapy versus chemotherapy alone for superior sulcus lung cancer. Lung Cancer 2018;122:206-13. [Crossref] [PubMed]
- . Postoperative radiotherapy in non-small-cell lung cancer: systematic review and meta-analysis of individual patient data from nine randomised controlled trials. PORT Meta-analysis Trialists Group. Lancet 1998;352:257-63. [Crossref] [PubMed]
- Burdett S, Stewart LPORT Meta-analysis Group. Postoperative radiotherapy in non-small-cell lung cancer: update of an individual patient data meta-analysis. Lung Cancer 2005;47:81-3. [Crossref] [PubMed]
- Burdett S, Rydzewska L, Tierney J, et al. Postoperative radiotherapy for non-small cell lung cancer. Cochrane Database Syst Rev 2016;10:CD002142 [Crossref] [PubMed]
- Billiet C, Decaluwé H, Peeters S, et al. Modern post-operative radiotherapy for stage III non-small cell lung cancer may improve local control and survival: a meta-analysis. Radiother Oncol 2014;110:3-8. [Crossref] [PubMed]
- Abuodeh Y, Naghavi AO, Echevarria M, et al. Quantitative excessive normal tissue toxicity and poor target coverage in postoperative lung cancer radiotherapy meta-analysis. Clin Lung Cancer 2018;19:e123-30. [Crossref] [PubMed]
- Isaka M, Kojima H, Takahashi S, et al. Risk factors for local recurrence after lobectomy and lymph node dissection in patients with non-small cell lung cancer: Implications for adjuvant therapy. Lung Cancer 2018;115:28-33. [Crossref] [PubMed]
- Zeng WQ, Feng W, Zhang CC, et al. Postoperative radiotherapy for resected stage IIIA-N2 non-small-cell lung cancer: a population-based time-trend study. Lung 2019;197:741-51. [Crossref] [PubMed]
- Liu T, Mu Y, Dang J, et al. The role of postoperative radiotherapy for completely resected pIIIA-N2 non-small cell lung cancer patients with different clinicopathological features: a systemic review and meta-analysis. J Cancer 2019;10:3941-9. [Crossref] [PubMed]
- Le Péchoux C, Dunant A, Pignon JP, et al. Need for a new trial to evaluate adjuvant postoperative radiotherapy in non-small-cell lung cancer patients with N2 mediastinal involvement. J Clin Oncol 2007;25:e10-e11. [Crossref] [PubMed]
- Keller SM, Adak S, Wagner H, et al. A randomized trial of postoperative adjuvant therapy in patients with completely resected stage II or IIIA non-small-cell lung cancer. Eastern Cooperative Oncology Group. N Engl J Med 2000;343:1217-22. [Crossref] [PubMed]
- Douillard JY, Rosell R, De Lena M, et al. Impact of postoperative radiation therapy on survival in patients with complete resection and stage I, II, or IIIA non-small-cell lung cancer treated with adjuvant chemotherapy: the adjuvant Navelbine International Trialist Association (ANITA) Randomized Trial. Int J Radiat Oncol Biol Phys 2008;72:695-701. [Crossref] [PubMed]
- Moreno AC, Haque W, Verma V, et al. Concurrent versus sequential chemoradiation therapy in completely resected pathologic N2 non-small cell lung cancer: Propensity-Matched analysis of the National Cancer Data Base. Ann Surg Oncol 2018;25:1245-53. [Crossref] [PubMed]
- Betticher DC, Hsu Schmitz SF, Tötsch M, et al. Prognostic factors affecting long-term outcomes in patients with resected stage IIIA pN2 non-small-cell lung cancer: 5-year follow-up of a phase II study. Br J Cancer 2006;94:1099-106. [Crossref] [PubMed]
- Amini A, Lou F, Correa A, et al. Predictors for locoregional recurrence for clinical stage III-N2 non-small cell lung cancer with nodal downstaging after induction chemotherapy and surgery. Ann Surg Oncol 2013;20:1934-40. [Crossref] [PubMed]
- Brandt WS, Yan W, Leeman JE, et al. Postoperative Radiotherapy for Surgically Resected ypN2 Non-Small Cell Lung Cancer. Ann Thorac Surg 2018;106:848-55. [Crossref] [PubMed]
- Billiet C, Peeters S, Decaluwé H, et al. Outcome after PORT in ypN2 or R1/R2 versus no PORT in ypN0 Stage III-N2 NSCLC after Induction Chemotherapy and Resection. J Thorac Oncol 2016;11:1940-53. [Crossref] [PubMed]
- Lee CY, Byun CS, Lee JG, et al. The prognostic factors of resected non-small cell lung cancer with chest wall invasion. World J Surg Oncol 2012;10:9. [Crossref] [PubMed]
- Drake JA, Sullivan JL, Weksler B. Adjuvant chemotherapy improves survival in patients with completely resected T3N0 non-small cell lung cancer invading the chest wall. J Thorac Cardiovasc Surg 2018;155:1794-802. [Crossref] [PubMed]
- Fernando HC, Landreneau RJ, Mandrekar SJ, et al. Impact of brachytherapy on local recurrence rates after sublobar resection: results from ACOSOG Z4032 (Alliance), a phase III randomized trial for high-risk operable non-small-cell lung cancer. J Clin Oncol 2014;32:2456-62. [Crossref] [PubMed]
- Califano R, Karamouzis MV, Banerjee S, et al. Use of adjuvant chemotherapy (CT) and radiotherapy (RT) in incompletely resected (R1) early stage Non-Small Cell Lung Cancer (NSCLC): a European survey conducted by the European Society for Medical Oncology (ESMO) young oncologists committee. Lung Cancer 2014;85:74-80. [Crossref] [PubMed]
- Smeltzer MP, Lin CC, Kong FS, et al. Survival impact of postoperative therapy modalities according to margin status in non-small cell lung cancer patients in the United States. J. Thorac Cardiovasc Surg 2017;154:661-672.e10. [Crossref] [PubMed]
- Hancock JG, Rosen JE, Antonicelli A, et al. Impact of adjuvant treatment for microscopic residual disease after non-small cell lung cancer surgery. Ann Thorac Surg 2015;99:406-13. [Crossref] [PubMed]
- Riquet M, Achour K, Foucault C, et al. Microscopic residual disease after resection for lung cancer: a multifaceted but poor factor of prognosis. Ann Thorac Surg 2010;89:870-5. [Crossref] [PubMed]
- Rieber J, Deeg A, Ullrich E, et al. Outcome and prognostic factors of postoperative radiation therapy (PORT) after incomplete resection of non-small cell lung cancer (NSCLC). Lung Cancer 2016;91:41-7. [Crossref] [PubMed]
- Wang EH, Corso CD, Rutter CE, et al. Postoperative radiation therapy is associated improved overall survival in incompletely resected stage II and III non-small-cell lung cancer. J Clin Oncol 2015;33:2727-34. [Crossref] [PubMed]
- Verma V, Moreno AC, Haque W, et al. Sequential versus concurrent chemoradiation therapy by surgical margin status in resected Non-small cell lung cancer. J Natl Compr Canc Netw 2018;16:508-16. [Crossref] [PubMed]
- Vallières E, Van Houtte P, Travis WD, et al. Carcinoma in situ at the bronchial resection margin? A review J Thorac Oncol 2011;6:1617-23. [Crossref] [PubMed]
- Vansteenkiste JF, De Leyn PR, Deneffe GJ, et al. Clinical prognostic factors in surgically treated stage IIIA-N2 non-small cell lung cancer: analysis of the literature. Lung Cancer 1998;19:3-13. [Crossref] [PubMed]
- Moretti L, Yu DS, Chen H, et al. Prognostic factors for resected non-small cell lung cancer with pN2 status: implications for use of postoperative radiotherapy. Oncologist 2009;14:1106-15. [Crossref] [PubMed]
- Ettinger DS, Aisner DL, Wood DE, et al. NCCN Guidelines Insights: Non-Small Cell Lung Cancer, Version 5.2018. J Natl Compr Canc Netw 2018;16:807-21. [Crossref] [PubMed]
- Lally BE, Detterbeck FC, Geiger AM, et al. The risk of death from heart disease in patients with non-small cell lung cancer who receive postoperative radiotherapy: analysis of the Surveillance, Epidemiology and End Results database. Cancer 2007;110:911-7. [Crossref] [PubMed]
- Kepka L, Bujko K, Orlowski TM, et al. Cardiopulmonary morbidity and quality of life in non-small cell lung cancer patients treated with or without postoperative radiotherapy. Radiother Oncol 2011;98:238-43. [Crossref] [PubMed]
- Zhang Y, Han A, Fu Z, et al. The dosimetric comparisons of CRT, IMRT, ARC, CRT+IMRT and CRT +ARC of postoperative radiotherapy in IIIA-N2 stage non-small-cell lung cancer patients. Biomed Res Int 2019;2019:8989241 [Crossref] [PubMed]
- Spoelstra FO, Senan S, Le Péchoux C, et al. Lung Adjuvant Radiotherapy Trial Investigators Group Variations in target volume definition for postoperative radiotherapy in stage III non-small-cell lung cancer: analysis of an international contouring study. Int J Radiat Oncol Biol Phys 2010;76:1106-13. [Crossref] [PubMed]
- Feng W, Fu XL, Cai XW, et al. Patterns of local-regional failure in completely resected stage IIIA (N2) non-small cell lung cancer cases: implications for postoperative radiation therapy clinical target volume design. Int J Radiat Oncol Biol Phys 2014;88:1100-7. [Crossref] [PubMed]
- Kępka L, Bujko K, Bujko M, et al. Target volume for postoperative radiotherapy in non-small cell lung cancer: results from a prospective trial. Radiother Oncol 2013;108:61-5. [Crossref] [PubMed]
- Nestle U, De Ruysscher D, Ricardi U, et al. ESTRO ACROP guidelines for target volume definition in the treatment of locally advanced non-small cell lung cancer. Radiother Oncol 2018;127:1-5. [Crossref] [PubMed]
(English Language Editor: J. Gray)


