Global trends of lung cancer mortality and smoking prevalence
Introduction
Before the start of mass production of tobacco products in the late 19th century, lung cancer was a rare cancer (1). Currently, however, it is the leading cause of cancer deaths in males and the second leading cause in females globally (2). In 2012, lung cancer killed an estimated 1,098,700 men and 491,200 women worldwide, corresponding to 24% and 14% of all cancer deaths in males and females, respectively (2).
The most important cause of lung cancer is tobacco smoking, although the proportion of lung cancer deaths attributable to smoking vary across populations, ranging from >80% in the United States (3) and France (4) to 61% in a pooled analysis of 21 Asian cohorts (5) and 40% in sub-Saharan Africa (6). Lung cancer is also caused by secondhand tobacco smoke, with an estimated 21,400 lung cancer deaths in non-smokers annually (7). Other risk factors for lung cancer include indoor air pollution because of unventilated combustion of coal in the household for heating and cooking (8); outdoor air pollution (9,10); exposure to hazardous chemicals in some occupations, such as coal gasification and aluminum production (11); exposure to radiation from indoor radon released from soil and building materials (12); and exposure to asbestos, silica dust, and several elements, including arsenic (13). Most of the lung cancer deaths due to secondhand smoke and indoor air pollution occur in low- and middle-income countries (LMICs), particularly China (14,15).
In this article, we present estimated worldwide lung cancer mortality rates in 2012. We also show trends of lung cancer mortality during recent decades in select countries in various global regions. Trends in lung cancer mortality rates in a country generally follow historical trends in smoking prevalence, with the trend in lung cancer rates lagging 20-30 years. Therefore, we present contemporary regional smoking prevalence and recent trends in order to provide insights into future lung cancer trends. We do not provide detailed information about the risk factors other than smoking because, except for some specific populations, these risk factors are responsible for a relatively small proportion of lung cancer deaths worldwide (14) and because data on these risk factors are sparse.
Data sources
We used GLOBOCAN 2012 as calculated by the International Agency for Research on Cancer (IARC) to provide estimates of lung cancer mortality rates for all countries worldwide (16). Estimates are generally of higher quality in high-income countries because of higher coverage and quality of death registration (17). We examined temporal trends in lung cancer rates for select countries using the World Health Organization (WHO) Mortality Database (18). All rates were age-standardized to the 1960 Segi world standard population and expressed per 100,000 population (19). We present data for mortality only because there are no substantial differences between incidence and mortality rates and trends, even in economically developed countries, because of poor survival (20). We used the United Nations groupings (with the exception of Cyprus, which is included in Southern Europe for GLOBOCAN) for the classification of the world’s regions (Table 1).
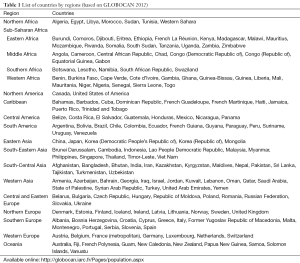
Full table
Data on smoking prevalence were obtained from The Tobacco Atlas, fifth edition (21), which used estimated data from the Institute for Health Metrics and Evaluation, University of Washington, United States (22), the WHO Report on the Global Tobacco Epidemic 2013 (23), and a national survey with more recent data that were not included in the above sources (24).
Lung cancer mortality rates in 2012
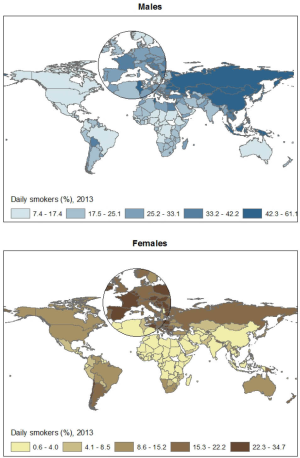
Lung cancer is the leading cause of cancer death in 87 countries in men and 26 countries in women, with the latter largely confined to high income countries (2). There is large variation in mortality rates across the world in both males and females (Figure 1), with about 30-fold difference in both sexes.
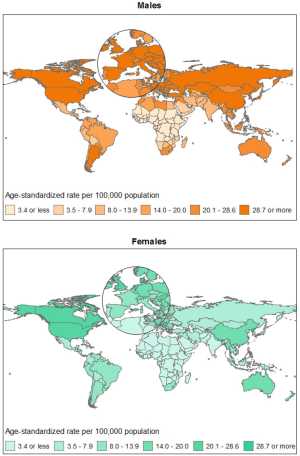
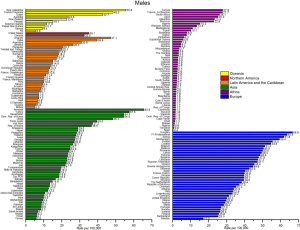
Among males, the highest rates (per 100,000) worldwide are found in Hungary (66.6), Armenia (65.6), the Former Yugoslav Republic of Macedonia (63.5), and Serbia (61.8) (Figure 2), whereas the lowest rates are found in Nigeria, Tanzania, and Niger (all <1.0). In general, the highest mortality rates (per 100,000) in males by region were in Central and Eastern Europe (47.6) and Eastern Asia (44.8) and the lowest rates are found in Northern Africa (14.0), South-Central Asia (10.7), Central America (9.0), and sub-Saharan Africa (4.4), with the lowest rate in Western Africa (1.5 per 100,000).
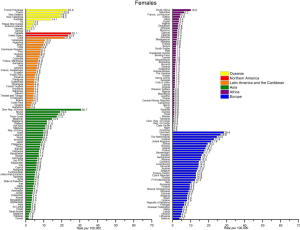
Among females, the highest lung cancer mortality rates (per 100,000) in 2012 worldwide were found in North Korea (30.7), Denmark (28.4), Hungary (26.6), and Canada (25.1) (Figure 3). By region, the highest estimated lung cancer mortality rates (per 100,000) in 2012 were in Northern America (23.5), Northern Europe (19.1), Eastern Asia (16.2), Western Europe (14.8), Oceania (14.1), and Caribbean (12.2). Apart from Eastern Asia, whose overall rates are dominated by China, in all these populations smoking prevalence in women has been moderate to high. The high mortality in China (18.0 per 100,000) despite a relatively lower prevalence of female smoking compared to more developed countries is likely due to higher exposure to secondhand smoke and indoor air pollution from unventilated combustion of coal used for heating and cooking purposes (8,14). Lung cancer mortality rates in women were the lowest in the regions where female smoking has been historically uncommon, including Western Asia (6.2 per 100,000), Central America (4.3 per 100,000), South-Central Asia (3.1 per 100,000), Northern Africa (2.8 per 100,000), and sub-Saharan Africa (2.2 per 100,000). The lowest estimated mortality rates were for Middle Africa (0.7 per 100,000).
Tobacco epidemic
In most high-income countries, smoking prevalence in men started to increase rapidly from the beginning of the 19th century (25,26). After a few decades, this increase was followed by a substantial increase in smoking prevalence in women (25,26). In the United States, the prevalence reached its peak in the 1950s in men (~55%) and in the 1960s in women (~35%). Changes in smoking prevalence in high-income countries have been reflected in smoking-related mortality by an approximately 3-4 decade lag (26). This pattern is commonly termed the ‘tobacco epidemic’ or ‘cigarette epidemic’. It should be noted that in a few high-income countries, including Japan, smoking prevalence did not increase in females following the increase in male smoking (27). Similarly, female smoking has not substantially increased in many LMICs, in particular Asian and African countries; however, a surge in male smoking in Asia has happened much more recently than in high-income countries and an increase in male smoking in many sub-Saharan African countries has started only lately.
In the process of tobacco epidemic, usually the average intensity of smoking (or the number of cigarettes smoked per day) increases while the age of smoking initiation decreases. The mean age of smoking initiation after the epidemic is established is generally <20 years, while it is usually higher before or in the earlier stages of the tobacco epidemic (3,28). Over time, an increase in smoking intensity, smoking initiation in earlier ages, or a combination of both can increase the magnitude of the association between smoking and lung cancer in a population. In the United States, the relative risk for the association between current smoking and lung cancer mortality in women increased from 2.7 to 12.7 and to 25.7 in cohorts conducted in the 1960s, 1980s, and 2000s, respectively (29).
There are substantial differences in smoking prevalence in socioeconomic groups in many countries. In high-income countries, smoking prevalence at the beginning of the tobacco epidemic (before the middle of the last century) in both men and women was highest in persons with higher socioeconomic status (30,31). Over time, in particular after the health effects of smoking became known in the 1950s and early 1960s, the high smoking prevalence shifted to lower socioeconomic groups as persons with higher socioeconomic status became more likely to quit and less likely to initiate smoking (32). In 1940 and 2009–2010, respectively, smoking prevalence in the United States in those with college education and above was 40% and 13%, whereas in those with less than high school education, it was 36% and 35%, respectively (31,32). In LMICs, similar changing patterns of smoking prevalence by socioeconomic status have been reported (33-35). Some ethnic groups have higher smoking prevalence in part because they are disproportionately represented in lower socioeconomic groups (36,37). Similar to patterns of smoking, mortality rates within a country are usually higher among lower socioeconomic groups.
Trends in smoking prevalence and lung cancer mortality rates by region
In 2012, an estimated 928 million men and 207 million women were current smokers (38). Currently, countries with the highest male smoking prevalence are generally in Eastern and South-Eastern Asia and Eastern Europe (Figure 4). European countries have the highest female smoking rates, followed by Oceania and Northern and Southern America.
There have been substantial variations in trends of smoking prevalence across countries (22). While many countries, notably high-income countries, have seen a considerable decrease in smoking prevalence in both males and females, in many other countries there has been little decrease or even an increase in smoking prevalence (21). Similarly, the lung cancer patterns vary across countries, from decreasing, stabilizing, and increasing in view of temporal trends in lung cancer rates which lag 3-4 decades following smoking trends (26).
Americas
In many countries in the Americas, smoking prevalence is approximately 20–30% in men and 10–20% in women, although prevalence is lower in most countries in Central America, especially among women. Following the start of a considerable decrease in male smoking prevalence from the 1950s and 1960s in the United States and Canada, lung cancer mortality rates in men have substantially dropped in both countries, from a peak of over 50 deaths per 100,000 in 1990 to about 30 deaths per 100,000 around 2010 (Figure 5). The decrease in smoking and lung cancer mortality among women in these two countries followed a similar pattern but with an approximately 20 years lag (Figure 6) (26).
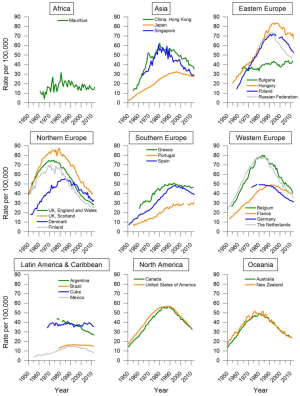
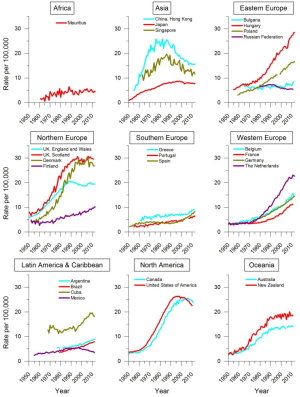
The tobacco epidemic in many South American and Caribbean countries began a few decades later than in Northern America, with the smoking prevalence first increasing in men and then in women. In most of these countries, smoking prevalence has decreased in both men and women, although the decreases were smaller and started later than in Northern America. There has been no significant decrease in smoking prevalence in a few countries in this region, including Chile, Costa Rica, Jamaica, Peru, and Suriname (22). Depending on whether or when smoking prevalence has started to decline in these countries, the lung cancer mortality trend is a mixture of decreasing (Argentina, Mexico) or stable (Brazil, Cuba) mortality rates in men (Figure 5), while in many countries it has been increasing in women (Argentina, Brazil) (Figure 6) (39).
Europe
Some Northern European countries have been able to substantially reduce smoking prevalence in both men and women (21). In these countries, lung cancer mortality rates in men have been decreasing for several decades, such as in the United Kingdom and Denmark (Figure 5), but among women, the mortality rate has just recently started to decrease in the United Kingdom and become stable in other countries (Figure 6), reflecting a later decline in smoking prevalence in women. Many other high-income countries in Europe, such as Germany and the Netherlands, have also seen a major decrease in prevalence of smoking in men, but with only a recent and modest decrease in female smoking (22). Consequently, lung cancer mortality rates in men in these countries have seen a substantial decrease in recent decades but they are still increasing in women. On the other hand, several countries in Eastern and Southern Europe and former republics of the Soviet Union have seen little/modest or very recent decreases in male smoking prevalence, and the prevalence is still high (generally, a daily smoking prevalence of ≥33%). In these countries, lung cancer mortality rates have been flat or increasing in men and increasing in women. Nevertheless, in many European countries in which the overall lung cancer mortality rates in women is increasing or stable, younger women (age 30–49 years) have seen a decrease in the mortality rates in more recent years, as this age group reflects the early effect of decreases in initiation of smoking (40).
Asia
Following an increase in smoking prevalence in most LMICs in Asia in the 1980s in men, the prevalence started to decrease in the mid-1990s in many of these countries, although the decrease has been mostly modest. However, smoking prevalence in men did not decrease in several countries in South-Eastern Asia (including Indonesia with male adult daily smoking prevalence of 57.1%, the highest in the world), Western Asia, and republics of the former Soviet Union in Central Asia (such as Kazakhstan, Turkmenistan, and Uzbekistan).
In higher-income populations of Asia, including Japan and Hong Kong (China), where male smoking prevalence surged and declined earlier than in other Asian countries, lung cancer mortality rates in men started a substantial decrease in the 1980s–1990s (Figure 5). Japan, Hong Kong (China), and Singapore have had some of the highest decreases in male smoking prevalence in Asia during 1980–2012 (41). In other high-income Asian countries, however, only a modest decrease in lung cancer mortality in South Korea from the 2000s (42,43) and an increase in Taiwan (44) have been reported.
Much less data on trends in lung cancer mortality are available from LMICs in Asia. However, patterns of male smoking prevalence suggest that lung cancer mortality among men in South-Eastern Asia and republics of the former Soviet Union in Central Asia are increasing and will stay high for several decades. In 2013, China had over 276 million daily smokers, of which 264 million were men (21). Following a substantial increase, China has seen a modest decrease in male smoking prevalence, with both the increase and decrease starting earlier in the urban population. Similarly, after an increase in lung cancer mortality rates in both the urban and rural populations of China, rates have started to slightly decline in the urban population, but they are still increasing in the rural population (45,46). In the remaining Asian LMICs, lung cancer mortality trends vary from increasing or stable to a modest decrease, depending on patterns of male smoking (47-51). Smoking in women in the majority of Asian LMICs has been traditionally low (mostly below 5%) and has changed little during 1980–2012 (22). Consequently, lung cancer mortality rates among women have been low and relatively stable in these countries (40), with an exception of some Asian countries, especially North Korea and China, where indoor air pollution appears to be an important risk factor for lung cancer in women. Notably, the lung cancer rate in Chinese women is higher than in many European countries with higher smoking prevalence, such as Germany, France, and Italy.
Africa
The overall smoking prevalence in African men is lower than in men from other parts of the world (Figure 4). With greater affordability of tobacco products, however, smoking prevalence in many sub-Saharan African countries has started to rise, and this increase has been predicted to continue if appropriate tobacco control interventions are not implemented (52). Information on trends of lung cancer mortality in Africa is sparse, but a few available epidemiological studies have suggested a decrease in lung cancer mortality among men in relatively higher income countries in Southern Africa (53), following a comprehensive tobacco control program including high tax on cigarettes (54). However, lung cancer mortality rates in men are expected to increase in many other African countries. Similar to Asia, smoking prevalence and lung cancer mortality among women in Africa has been low.
Oceania
Australia and New Zealand are among the few countries, along with the US and the UK, where the tobacco epidemic was first established (at the early part of the last century). Smoking prevalence substantially decreased in both sexes in recent decades (to <20% in 2013); consequently, lung cancer mortality rates in these countries have been decreasing in men and stabilizing in women (Figures 5,6). Smoking prevalence among men in some other countries in this region is generally high, and these countries are among some of the countries with highest lung cancer mortality rates worldwide (Figure 2). Although in several of these countries female smoking prevalence is <5%, in several others it is >10%, resulting in a wide variation in lung cancer mortality rates in females across the countries (Figure 3). Most of these countries have seen little change or modest decreases in smoking prevalence in recent decades (22).
Future perspectives
Lung cancer could be cured if it is diagnosed in early stages and if appropriate treatment is accessible. Low-dose computed tomographic screening of high-risk individuals for early detection of lung cancers could improve prognosis of lung cancer in this group (55,56), although this screening method has not been studied outside of high-income countries. Nevertheless, the best practice to reduce the burden of lung cancer is to prevent it, because even the most successful screening programs would avert only a subset of all lung cancer deaths (this has been estimated to be ~8% in the US) (57), and the treatment of lung cancer is complicated and may not be accessible to everybody, particularly in low-resource countries. As the majority of lung cancer cases can be attributed to smoking, the main priority is to reduce smoking prevalence through effective tobacco control policies and regulations. Tobacco control policies averted an estimated number of over 800,000 premature deaths from lung cancer only in the US from 1975 to 2000 (58), despite wide variations in implementation of these policies across states. In the US, tobacco control policies are implemented at the state level, and southern states generally have less intense tobacco control and consequently higher smoking prevalence than other states (37). Tobacco control could not only reduce lung cancer mortality, but also lower the burden of multiple other smoking-related diseases. It has been shown that few public health investments provide greater dividends than tobacco control (21).
The WHO’s Framework Convention on Tobacco Control is a basis for countries to implement tobacco control policies and is an effective tool to reduce smoking prevalence and related harms (59). In order to facilitate implementation of these policies in countries, WHO has introduced MPOWER measures, which include (I) monitoring tobacco use and prevention policies; (II) smoke-free air policies; (III) cessation programs; (IV) warnings (health warnings and mass media); (V) bans on advertising, promotion, and sponsorship; and (VI) raising tobacco taxes (60). These policies can be implemented at increasing levels. Despite great achievements in tobacco control in a number of countries, the global coverage of the policies is still far behind the recommended levels by WHO. For example, out of 194 countries in the WHO’s list, only 29 countries have complete tobacco advertising ban policies, 71 countries have moderate to complete smoke-free policies, and 49 countries (with approximately 20% of the world’s population) are covered by at least two policies at the highest level (60). In 2012, Turkey became the first (and so far the only) country that has achieved the highest level of all six MPOWER measures (61,62). Iran, Panama, and Uruguay are the countries that have achieved the highest level of recommended for five measures (all measures except for taxation) (63).
A major priority for most LMICs is to prevent the tobacco epidemic in women, and for most sub-Saharan African countries is to prevent a surge in smoking in both sexes. In addition to local funding, international aid could help tobacco control programs being implemented in very low-resource countries. In addition to tobacco control, efforts should be made to reduce the exposure to other risk factors of lung cancer, notably indoor and outdoor air pollution, when applicable.
Conclusions
Despite major achievements in tobacco control, with current smoking patterns lung cancer will remain a major cause of death worldwide for several decades. Effective tobacco control policies must be implemented or enforced in order to further reduce smoking prevalence. Lung cancer mortality is likely to greatly increase in sub-Saharan Africa if appropriate tobacco control programs are not implemented. Although smoking is a highly preventable risk factor for lung cancer, exposure to other risk factors (e.g., indoor and outdoor air pollution) also needs to be reduced, when applicable.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have declared no conflicts of interest.
References
- Herbert H. A Case of Primary Carcinoma of the Lung. Cal State J Med 1905;3:143-4. [PubMed]
- Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA Cancer J Clin 2015;65:87-108. [PubMed]
- National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2014.
- Ribassin-Majed L, Hill C. Trends in tobacco-attributable mortality in France. Eur J Public Health 2015. [Epub ahead of print]. [PubMed]
- Zheng W, McLerran DF, Rolland BA, et al. Burden of total and cause-specific mortality related to tobacco smoking among adults aged ≥ 45 years in Asia: a pooled analysis of 21 cohorts. PLoS Med 2014;11:e1001631. [PubMed]
- Institute for Health Metrics and Evaluation (IHME). GBD Cause Patterns. Available online: http://vizhub.healthdata.org/gbd-cause-patterns/, accessed on Jul 28, 2015.
- Oberg M, Jaakkola MS, Woodward A, et al. Worldwide burden of disease from exposure to second-hand smoke: a retrospective analysis of data from 192 countries. Lancet 2011;377:139-46. [PubMed]
- Secretan B, Straif K, Baan R, et al. A review of human carcinogens--Part E: tobacco, areca nut, alcohol, coal smoke, and salted fish. Lancet Oncol 2009;10:1033-4. [PubMed]
- Hamra GB, Guha N, Cohen A, et al. Outdoor particulate matter exposure and lung cancer: a systematic review and meta-analysis. Environ Health Perspect 2014;122:906-11. [PubMed]
- Loomis D, Grosse Y, Lauby-Secretan B, et al. The carcinogenicity of outdoor air pollution. Lancet Oncol 2013;14:1262-3. [PubMed]
- Baan R, Grosse Y, Straif K, et al. A review of human carcinogens--Part F: chemical agents and related occupations. Lancet Oncol 2009;10:1143-4. [PubMed]
- El Ghissassi F, Baan R, Straif K, et al. A review of human carcinogens--part D: radiation. Lancet Oncol 2009;10:751-2. [PubMed]
- Straif K, Benbrahim-Tallaa L, Baan R, et al. A review of human carcinogens--Part C: metals, arsenic, dusts, and fibres. Lancet Oncol 2009;10:453-4. [PubMed]
- Sisti J, Boffetta P. What proportion of lung cancer in never-smokers can be attributed to known risk factors? Int J Cancer 2012;131:265-75. [PubMed]
- Hashim D, Boffetta P. Occupational and environmental exposures and cancers in developing countries. Ann Glob Health 2014;80:393-411. [PubMed]
- Ferlay J, Soerjomataram I, Ervik M, et al. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11 [Internet]. Lyon, France: International Agency for Research on Cancer. Available online: http://globocan.iarc.fr
- Mathers CD, Fat DM, Inoue M, et al. Counting the dead and what they died from: an assessment of the global status of cause of death data. Bull World Health Organ 2005;83:171-7. [PubMed]
- World Health Organization. WHO Mortality Database. Available online: http://www.who.int/healthinfo/statistics/mortality_rawdata/en/index.html, accessed on May 28, 2015.
- Segi M. Cancer mortality for selected sites in 24 countries (1950-57). Sendai: Dept. of Public Health, Tohoku University School of Medicine, 1960.
- Jemal A, Thun MJ, Ries LA, et al. Annual report to the nation on the status of cancer, 1975-2005, featuring trends in lung cancer, tobacco use, and tobacco control. J Natl Cancer Inst 2008;100:1672-94. [PubMed]
- Eriksen MP, Mackay J, Schluger N, et al. The tobacco atlas. 5th ed. Atlanta: American Cancer Society, 2015.
- Ng M, Freeman MK, Fleming TD, et al. Smoking prevalence and cigarette consumption in 187 countries, 1980-2012. JAMA 2014;311:183-92. [PubMed]
- World Health Organization. WHO Report on the Global Tobacco Epidemic, 2013: Enforcing bans on tobacco advertising, promotion and sponsorship. Geneva, Switzerland, 2013.
- Australian Institute of Health and Welfare. NDSHS 2013 data & references. Available online: http://www.aihw.gov.au/alcohol-and-other-drugs/ndshs/2013/data-and-references/
- Lopez AD, Collishaw NE, Piha T. A descriptive model of the cigarette epidemic in developed countries. Tob Control 1994;3:242-7.
- Thun M, Peto R, Boreham J, et al. Stages of the cigarette epidemic on entering its second century. Tob Control 2012;21:96-101. [PubMed]
- Funatogawa I, Funatogawa T, Yano E. Trends in smoking and lung cancer mortality in Japan, by birth cohort, 1949-2010. Bull World Health Organ 2013;91:332-40. [PubMed]
- Giovino GA, Mirza SA, Samet JM, et al. Tobacco use in 3 billion individuals from 16 countries: an analysis of nationally representative cross-sectional household surveys. Lancet 2012;380:668-79. [PubMed]
- Thun MJ, Carter BD, Feskanich D, et al. 50-year trends in smoking-related mortality in the United States. N Engl J Med 2013;368:351-64. [PubMed]
- Graham H. Smoking prevalence among women in the European community 1950-1990. Soc Sci Med 1996;43:243-54. [PubMed]
- De Walque D. Education, information, and smoking decisions: evidence from smoking histories, 1940-2000. The World Bank Web site: http://elibrary.worldbank.org/doi/book/10.1596/1813-9450-3362
- Garrett BE, Dube SR, Winder C, et al. Cigarette smoking - United States, 2006-2008 and 2009-2010. MMWR Surveill Summ 2013;62 Suppl 3:81-4. [PubMed]
- Hiscock R, Bauld L, Amos A, et al. Socioeconomic status and smoking: a review. Ann N Y Acad Sci 2012;1248:107-23. [PubMed]
- Bosdriesz JR, Mehmedovic S, Witvliet MI, et al. Socioeconomic inequalities in smoking in low and mid income countries: positive gradients among women? Int J Equity Health 2014;13:14. [PubMed]
- Sreeramareddy CT, Pradhan PM, Mir IA, et al. Smoking and smokeless tobacco use in nine South and Southeast Asian countries: prevalence estimates and social determinants from Demographic and Health Surveys. Popul Health Metr 2014;12:22. [PubMed]
- Sitas F, Egger S, Bradshaw D, et al. Differences among the coloured, white, black, and other South African populations in smoking-attributed mortality at ages 35-74 years: a case-control study of 481,640 deaths. Lancet 2013;382:685-93. [PubMed]
- Islami F, Ward EM, Jacobs EJ, et al. Potentially preventable premature lung cancer deaths in the USA if overall population rates were reduced to those of educated whites in lower-risk states. Cancer Causes Control 2015;26:409-18. [PubMed]
- World Health Organization. World Health Statistics 2014. Available online: http://apps.who.int/iris/bitstream/10665/112738/1/9789240692671_eng.pdf, accessed on Jul 28, 2015.
- Chatenoud L, Bertuccio P, Bosetti C, et al. Trends in mortality from major cancers in the Americas: 1980-2010. Ann Oncol 2014;25:1843-53. [PubMed]
- Torre LA, Siegel RL, Ward EM, et al. International variation in lung cancer mortality rates and trends among women. Cancer Epidemiol Biomarkers Prev 2014;23:1025-36. [PubMed]
- Mackay J, Ritthiphakdee B, Reddy KS. Tobacco control in Asia. Lancet 2013;381:1581-7. [PubMed]
- Chung JI, Song YM, Choi JS, et al. Trends in avoidable death over 20 years in Korea. J Korean Med Sci 2008;23:975-81. [PubMed]
- Jung KW, Shin HR, Kong HJ, et al. Long-term trends in cancer mortality in Korea (1983-2007): a joinpoint regression analysis. Asian Pac J Cancer Prev 2010;11:1451-7. [PubMed]
- Chen BK, Yang CY. Temporal trend analysis of avoidable mortality in Taiwan, 1971-2008: overall progress, with areas for further medical or public health investment. BMC Public Health 2013;13:551. [PubMed]
- Yang L, Parkin DM, Li L, et al. Time trends in cancer mortality in China: 1987-1999. Int J Cancer 2003;106:771-83. [PubMed]
- Guo P, Huang ZL, Yu P, et al. Trends in cancer mortality in China: an update. Ann Oncol 2012;23:2755-62. [PubMed]
- Sriplung H, Wiangnon S, Sontipong S, et al. Cancer incidence trends in Thailand, 1989-2000. Asian Pac J Cancer Prev 2006;7:239-44. [PubMed]
- Moradpour F, Fatemi Z. Estimation of the projections of the incidence rates, mortality and prevalence due to common cancer site in Isfahan, Iran. Asian Pac J Cancer Prev 2013;14:3581-5. [PubMed]
- Al-Hashimi MM, Wang XJ. Trend analysis of lung cancer incidence rates in ninawa province, Iraq, from 2000 to 2010--decrease and recent stability. Asian Pac J Cancer Prev 2014;15:385-90. [PubMed]
- Wani MA, Jan FA, Khan NA, et al. Cancer trends in Kashmir; common types, site incidence and demographic profiles: National Cancer Registry 2000-2012. Indian J Cancer 2014;51:133-7. [PubMed]
- Keyghobadi N, Rafiemanesh H, Mohammadian-Hafshejani A, et al. Epidemiology and trend of cancers in the province of Kerman: southeast of Iran. Asian Pac J Cancer Prev 2015;16:1409-13. [PubMed]
- Blecher E, Ross H. Tobacco use in Africa: Tobacco control through prevention. Atlanta: American Cancer Society, 2013.
- Parkin DM, Bray F, Ferlay J, et al. Cancer in Africa 2012. Cancer Epidemiol Biomarkers Prev 2014;23:953-66. [PubMed]
- Reddy P, James S, Sewpaul R, et al. A decade of tobacco control: the South African case of politics, health policy, health promotion and behaviour change. S Afr Med J 2013;103:835-40. [PubMed]
- National Lung Screening Trial Research Team, Aberle DR, Adams AM, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011;365:395-409. [PubMed]
- Moyer VA; U.S. Preventive Services Task Force. Screening for lung cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2014;160:330-8. [PubMed]
- Ma J, Ward EM, Smith R, et al. Annual number of lung cancer deaths potentially avertable by screening in the United States. Cancer 2013;119:1381-5. [PubMed]
- Moolgavkar SH, Holford TR, Levy DT, et al. Impact of reduced tobacco smoking on lung cancer mortality in the United States during 1975-2000. J Natl Cancer Inst 2012;104:541-8. [PubMed]
- Islami F, Stoklosa M, Drope J, et al. Global and regional patterns of tobacco smoking and tobacco control policies. Eur Urol Focus 2015.
- World Health Organization. WHO report on the global tobacco epidemic, 2015: Raising taxes on tobacco—Executive summary. Available online: http://apps.who.int/iris/bitstream/10665/178577/1/WHO_NMH_PND_15.5_eng.pdf?ua=1&ua=1&ua=1, accessed on Jul 28, 2015.
- Campaign for Tobacco-Free Kids. Tobacco tax success story: Turkey. Available online: http://www.fctc.org/images/stories/success_Turkey_en.pdf, accessed on Jul 28, 2015.
- World Health Organization. WHO report on the global tobacco epidemic, 2015: Raising taxes on tobacco— Appendix I: Regional summary of MPOWER measures. Available online: http://www.who.int/tobacco/global_report/2015/appendix1.pdf?ua=1, accessed on Jul 28, 2015.
- World Health Organization. WHO report on the global tobacco epidemic, 2015: Raising taxes on tobacco— Appendix III: Year of highest level of achievment in selected tobacco control measures. Available online: http://www.who.int/tobacco/global_report/2015/appendix3.pdf?ua=1, accessed on Jul 28, 2015.


