
Has programmed cell death ligand-1 MET an accomplice in non-small cell lung cancer?—a narrative review
Introduction
Non-small cell lung cancer (NSCLC; 80–85% of all lung cancers) continues to be one of the major causes of cancer related deaths around the world (1). The development of approved molecularly targeted therapies (small molecules) has, however, significantly improved outcomes in the metastatic setting for NSCLC patients harbouring activated oncogenes such as epidermal growth factor receptor (EGFR), translocated anaplastic lymphoma kinase (ALK), ROS-oncogene-1 (ROS-1), rapidly accelerated fibrosarcoma B (B-raf), and mesenchymal-epithelial transition c (c-MET) (2). By targeting the main pathways of NSCLC signal transduction, these drugs dramatically improved progression-free survival (PFS) and quality of life (QoL) in this highly selected respective subgroup of NSCLC patients sparing them from toxic chemotherapy approaches.
In addition, it remains to be seen whether combinations of tyrosine kinase inhibitors (TKIs) with immune check-point inhibitors (CPIs) such as cytotoxic T lymphocyte antigen 4 (CTLA-4), programmed cell death 1 (PD-1) receptor and programmed cell death 1 ligand (PD-L1) might change current treatment paradigms in all NSCLCs (3,4). Only the identification of validated prognostic or predictive markers of response could help oncologists in choosing the most effective treatment (TKIs vs. chemotherapy vs. immunotherapy vs. combinations) for NSCLC patients.
Most recently, two novel highly selective oral c-MET exon 14 skipping mutation inhibitors (i.e., capmatinib and tepotinib) have been approved for NSCLC patients harbouring this c-MET mutation, however, the cross-talk between c-MET mutations, PD-L1 expression, and response to CPIs is still controversial and not fully understood.
In order to summarise the current knowledge, for this narrative review a comprehensive literature search using the following terms was conducted: c-MET mutations, c-MET amplification, PD-L1, prognostic value, NSCLC. For this search the following databases were included: PubMed database, Medline, Embase, Web of Science, and abstracts and posters presented at various scientific meetings (e.g., AACR, ASCO, ASH) from January 2000 through March 2021. We present the following article in accordance with the Narrative Review reporting checklist (available at http://dx.doi.org/10.21037/tlcr-21-124).
c-MET—signaltransduction pathways
The receptor tyrosine kinase c-MET and its ligand hepatocyte growth factor (“scatter factor”, HGF) is a well established cell surface receptor. c-MET is expressed in a bundle of different cell types (haematopoietic, epithelial, neuronal cells as well as malignant cells). Several lines of evidence have demonstrated that activation of the HGF/c-MET signaltansduction pathway contributes to the malignant phenotype by increasing cell proliferation, angiogenesis, migration, invasion, metastasis, and finally cell survival (5). In addition, c-MET has been shown to be a major resistance mechanism for EGFR-targeting agents, and HGF was found to enhance chemo- and radioresistance (6).
The c-MET receptor consists of a 45 kDa extracellular α-chain, linked to a 145 kDa transmembrane β-chain via disulphide bonds. After HGF binding, two MET receptors dimerise leading to autophosphorylation of three tyrosine residues (Y1230, Y1234, Y1235) (7). Following this initial phosphorylation cascade, additional phosphorylation of two other tyrosine residues (Y1349, Y1356) occurs (8,9) which results in a subsequent recruitment of signaling molecules such as SHC1 (comprised of three proteins with 66, 52, and 46 kD molecular weight) and Grb2 (growth factor receptor bound protein 2)/Gab2 (GrB2-associated binding protein). These proteins then form a complex which serves as docking site for SHP-2 (SH2 domain-containing phosphatases 2) for downstream signaling molecules (e.g., ras/raf, Akt/mTOR etc.) [reviewed by (10)].
So far, several mechanisms have been identified how the c-MET receptor can be activated including interaction with its ligand HGF, genomic amplification, receptor-protein overexpression, point mutations, alternative splicing, and probably also by chromosomal translocation (11).
c-MET exon 14 alterations (point mutations, deletions, insertions, and complex mutations) lead to decreased degradation of c-MET receptor, resulting in the activation of c-MET signaling and the tumorigenesis (12), and impaired c-MET receptor degradation seems to be a mechanism for ligand-independent aberrant MET signaling (13).
Interestingly, in NSCLCs nearly all of the c-MET exon 14 skipping mutations can delete Y1003 (the c-cbl binding site) in the juxtamembrane domain (14,15). This leads to c-MET ubiquitination abrogation, increased c-MET protein stability, and impaired c-MET degradation which then, in turn, induces ligand-independent c-MET activation (13,14).
c-MET—immunotherapy resistance
c-MET alterations and PD-L1 expression
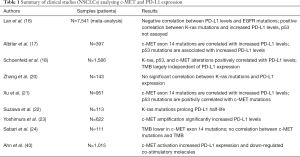
Several lines of evidence have demonstrated that harbouring altered c-MET in NSCLC patients is associated with lower overall response rates (ORRs) and shorter PFS than in tumours without such mutations. Collectively altered c-MET is thought to be associated with a significantly higher PD-L1 expression (16-19).
In an attempt to further explore the relationship between c-MET and PD-L1 expression in NSCLCs, Albitar and co-workers (17) retrospectively analysed 397 lung cancers in terms of c-MET, p53, K-ras and EGFR. They found that PD-L1 expression was negatively correlated with EGFR mutations (P=0.0003), and positively correlated with p53 mutations (P=0.0001) and c-MET amplification (P=0.004). Moreover, patients with p53 mutations had significantly higher c-MET amplification (P=0.007), and were more likely (P=0.0002) to have an EGFR wild type. Interestingly, there was no correlation between K-ras mutations and PD-L1 expression detected, however, a significant positive correlation between PD-L1 expression and K-ras with a p53 co-mutation was discovered (P=0.0002). Although in a few smaller studies a correlation between K-ras and PD-L1 expression was seen (20), this study could not confirm this finding. Finally, patients harbouring p53 mutations had a much higher PD-L1 expression level when compared with wild-type p53 suggesting that c-MET in conjunction with p53 triggers the observed up-regulation of PD-L1 levels.
Similar findings have been detailed by a Chinese group of researchers (21) in their NSCLC cohort study (N=951). Using an RNA-based sequencing method, they found that PD-L1 expression in patients harbouring c-MET exon 14 skipping mutations was significantly higher when compared with the c-MET wild-type (69.2% vs. 17.3%, P<0.01) and the PD-L1 expression was found to be significantly lower in the EGFR mutant cohort when compared with the wild-type (9.3% vs. 26.9%, P<0.01). Again, p53 mutations were found in 37.5% of all patients harbouring a c-MET exon 14 skipping mutation.
Clinical data from 113 NSCLC patients also shed some light on the relationship of K-ras and c-MET. Suzawa et al. (22) provided the first evidence that expression of mutated K-ras proteins prolonged the half-life of the mutated c-MET exon 14 protein. Trametinib, however, was found to down-regulate c-MET exon 14 expression under these experimental conditions which was associated with a loss of phosphorylation (23) suggesting that K-ras might be the master regulator of alterated c-MET.
Further evidence was provided by Lan et al. (16) who conducted a meta-analysis to investigate the relationship between PD-L1 expression and driver gene mutations in NSCLC patients. In this meta-analysis a total of 26 studies with 7,541 patients were analysed. Using a random effect model, a significant negative correlation was found between PD-L1 expression and EGFR mutations (P=0.014), whereas a positive correlation between K-ras mutations and PD-L1 up-regulation was seen (P=0.001). The mutation status of p53, however, has not been analysed. The authors could not detect a correlation between c-MET expression levels and PD-L1 (P=0.298), however, this might be due to the fact that only two c-MET-related studies were included for this subanalysis.
Correlation between c-MET and PD-L1 expression
Most recently, Yoshimura and co-workers (23) attempted to correlate c-MET amplification with PD-L1 expression and tumour-infiltration lymphocytes (TILs) in the surrounding tumour tissue in 622 resected tumour specimens. c-MET amplification was assayed using the FISH methodology while PD-L1 expression was analysed using immuno-histochemistry. In line with many other investigators, they found that PD-L1 expression was significantly increased in tumours with c-MET amplifications (P=0.019). Surprisingly, in these tumours also a significant increase of TILs (mainly CD8-positive CTLs) was detected. From this study it was concluded that only c-MET amplifications are implicated in the inflamed tumour microenvironment suggesting that NSCLCs harbouring c-MET amplifications are responsive to CPI therapies. A similar study with c-MET exon 14 mutations has not yet been conducted.
An experimental study with a slightly different design has been published most recently by Schoenfeld et al. (18). For 1,586 NSCLC patients (adenocarcinomas) paired PD-L1 testing and targeted next-generation sequencing was performed in the primary tumour and in metastatic samples. PD-L1 subgroups were defined as negative (PD-L1 <1%), intermediate (PD-L1 =1–49%), and high (PD-L1 ≥50%). Distribution of PD-L1 expression was found to be 66.6% (negative), 17.9% (intermediate), and 15.5% (high) with PD-L1 expression not significantly differing by age, sex, or smoking status.
In line with other major studies, mutations of K-ras, p53, and c-MET were significantly positively correlated with high PD-L1 expression (P<0.001 for each), whereas EGFR mutations were found to be significantly associated with PD-L1 negativity (P=0.005). Interestingly, the researchers found that PD-L1 expression was significantly lower in the primary tumour when compared with the metastatic site (P<0.001), and amongst all metastatic sites the highest degree of PD-L1 expression was seen in lymph nodes (PD-L1 high =30%) and least in bone deposits (PD-L1 high =16%). Of note, only 20% of brain metastases (total N=61) were found to express high PD-L1 levels, the vast majority of samples were PD-L1 negative. In this study the authors also measured tumour mutational burden (TMB) and found that TMB appeared to be largely independent of the PD-L1 status. This study, which is to date the largest series of lung adenocarcinomas, finally confirmed the general observation that c-MET alterations are associated with increased PD-L1 levels and may, therefore, pave the way for better combination studies in the near future.
Involvement of TMB and TME
TMB levels have also been analysed in a separate but smaller study (24). In 111 evaluable NSCLC specimens with c-MET exon 14 skipping mutations, TMB levels were measured. The mean TMB was lower in the c-MET mutated group when compared with unselected NSCLC patients (3.8 vs. 5.7 mutations/megabase, P<0.001). Although c-MET mutated tumours expressed PD-L1, a correlation with TMB was not detected and neither PD-L1 status nor TBM correlated with treatment response. These finding may add weight to the proposal that PD-L1 should be regarded to be a biological continuum and, therefore, might be of limited value as a biomarker in this subset of patients (4).
The tumour microenvironment (TME) is the nest where interactions between tumour cells and the immune system take place and might, therefore, be amenable for therapeutic interactions. The TME is known to be a complex tissue structure which contains cancer-associated fibroblasts (CAFs), tumour-associated macrophages (TAMS), blood vessels, and several immune cells (e.g., T cells, neutrophils, etc.). Of note, the TME can also contribute to tumorigenesis, progression, therapy resistance, and metastatic spread (25). Of special interest are TAMs (expressing PD-L1, CD33, and CD163). Although TAMs (the main component of the TME) belong to the group of antigen-presenting cells (APCs), their ability to present tumour antigens is very limited (massive down-regulation of CD80/CD86 and MHC-I/II expression). Via PD-L1 on their cell surface they act as immunosuppressive cells and are also able to stimulate PD-1-positive Tregs (26).
Interestingly, it has been demonstrated the HGF (c-MET ligand) is secreted in a paracrine manner by fibroblasts in the TME, and not by the tumor cells themselves (27).
In addition, M1-polarised macrophages (Th1-associated) mediate tumour cell death while the M2 macrophages (Th2-associated) promote tumour growth. Stimulation of macro-phages with HGF results in differentiation of M1 macrophages to M2 subtypes (28), underscoring the functional relevance of HGF/MET axis in the antitumor immune response.
The role of the TME in correlation with the HGF/c-MET axis has been highlighted recently in two experimental studies. Benkhoucha et al. (29) provided the first evidence that HGF appears to be a potent immunomodulatory molecule that can inhibit dendritic cells (DCs) and down-regulate tumour-killing T cells. In addition, the observed effects could be fully reversed when DCs were pre-treated with anti-c-MET antibodies. Although c-MET is not expressed in CD4-positive and CD8-positive T cells, the effect is still remarkable.
In line with these findings are results provided by Glodde et al. (30). Using a human malignant melanoma mouse model, the authors demonstrated that HGF/c-MET signaling can mobilise neutrophils to tumours and lymph nodes following cancer immunotherapies. In addition, in T cell-inflamed tumour tissues these c-MET-positive neutrophils rapidly acquire immunosuppressive properties (similar to TAMs) and can suppress T cell expansion and CD8-positive cytotoxic T cells. In cancer patients, high HGF levels were found which correlated with increasing neutrophil counts and poor CPI response (30). However, adding of a specific c-MET inhibitor (capmatinib) decreased neutrophils in the TME and enhanced cytotoxic T cells (CTLs) and other T effector cells. In addition, the authors could show for the first time that c-MET inhibition was able to alter the phenotype of CD8-positive cells. Following capmatinib exposure only very few CTLs expressed KLRG1 (killer cell lectin-like receptor G1) which is regarded to be a CD8+ T cell senescence marker indicative of reduced proliferative capacity (31) and, therefore, might serve as a putative biomarker in this experimental setting.
Both studies add weight to the proposal that under these experimental conditions c-MET expression can modulate the TME and thus tumour immune responses, a finding, that, if confirmed in other tumour models, will have major implication for combining c-MET inhibitors and CPIs.
GSK3β is a key player
The correlation between the expression of c-MET and PD-L1 has been extensively studied using a murine HCC model. Li and co-workers (31) demonstrated that c-MET inhibition was associated with PD-L1 upregulation. Furthermore, the combination of c-MET inhibitors (tivantinib, capmatinib) and a PD-1 inhibitor resulted in significant tumour regression and prolonged survival. Interestingly, it was also shown that c-MET directly phosphorylated glycogen synthase 3β (GSK3β) which activated the enzyme by preventing it from GSK3β ubiquitination and resulted in decreased PD-L1 expression (32). It was concluded that high c-MET expression is associated with increased GSK3β protein levels and low PD-L1 expression on the surface of murine HCC cells.
GSK3β, a serine-threonine kinase, has the highest number of substrates and many roles in maintaining the cellular functions including immune response. The enzyme is normally not altered at a genomic level (e.g., amplifications, mutations) which might explain, at least in part, why no specific inhibitors have been identified so far (33). Initially, GSK3β has been shown to negatively regulate the Wnt/β-catenin pathway by phosphorylation and subsequent degradation of β-catenin [reviewed by (34)]. However, more recent research revealed that GSK3β is also a key player for the regulation of the PD-1/PD-L1 pathway in malignant cells by interacting with CD8-positive T cells (35). Moreover, GSK3β inhibition led to NFAT (nuclear factor of activated T cells 2) accumulation in T cells resulting in a significant T cell proliferation including Tregs (36).
Interestingly, PD-L1 is also known to be a substrate for GSK3β resulting in a number of different phosphorylation steps with final ubiquitination in the 26S proteasome (37). By contrast, PD-L1 glycosylation of residues N192, N200, and N219 has been shown to prevent GSK3β binding resulting in PD-L1 stabilisation (38). Of note, mutated EGFR (via AKT activation can also stablise PD-L1 via GSK3β inactivation which then can be reversed by anti-EGFR tyrosine kinase inhibitors (38).
Further evidence for the role of GSK3β has been provided by Sun et al. (39) in a landmark study. They exposed human lung cancer cell lines to the c-MET inhibitor tivantinib and could show that this increased PD-L1 levels and, in turn, made cells more resistant to T cell killing. Moreover, they also demonstrated that this finding was attributed to a c-MET-induced GSK3β suppression resulting in a stabilisation of PD-L1 levels. In turn, this allowed tumour cells to escape from CD8-positive T cell killing (40). From these novel findings it was concluded that the observed cross-talk between c-MET and PD-L1 might provide a rationale for combining both agents in clinical trials. Moreover, it is also conceivable that these observations, if confirmed, may explain, at least in part, the failure of certain c-MET inhibitors in NSCLC clinical trials.
Cross-talk between c-MET and PD-L1
It should be noted that the described putative cross-talk between c-MET activation and PD-L1 expression is not fully understood. By contrast, Ahn et al. (40) most recently provided compelling evidence in their experimental study that a significant positive correlation between c-MET and PD-L1 expression in NSCLC patients (N=1,015) exists, based on both, immunohistochemistry and TCGA (The Cancer Genome Atlas) analyses. Activation of c-MET can occur by gene amplification (41) which results in an overexpression of the c-MET protein (22–75% of NSCLC patients). In addition, mutations can also be detected (Table 1). A somatic mutation at position exon 14 splice junction leads to exon deletion and, in turn, to an altered protein that lacks the juxtamembrane domain which is the cause for a sustained c-MET activation (12). When looking at these alterations in their study, it was found that c-MET activation up-regulated PD-L1 and down-regulated co-stimulatory molecules such as CD137, CD252, CD70, and ICAM-1. Finally, from this study the authors concluded that c-MET alterations (e.g., amplifications and mutations) exert an immunosuppressive effect in the microenvironment of the tumours.
Full table
As described earlier several studies showed an inconsistent correlation between c-MET alterations and PD-L1 expression, and it is far from being clear how c-MET directly regulates PD-L1 expression in different cancers. Although it is generally accepted that c-MET alterations positively correlate with PD-L1 expression in NSCLCs, this is no not in RCC and HCC cells. PD-L1 is likely regulated by multiple factors, which are differentially activated in different cancer types and/or tissues. The findings provided by Li et al. (37) provide a plausible explanation for the poor results of c-MET inhibitors in HCC trials since inhibition of c-MET increased GSK3β levels which resulted in stabilisation of PD-L1 and allowed tumour cells to escape from immuno-surveillance. However, it should be noted that the study was performed in nu/nu mice, and human HCC samples were not analysed.
It is generally accepted that PD-L1 expression in tumour cells can be significantly induced by interferon-γ (IFN-γ) (most potent inducer) although other cytokines may have also some effects (42), which explains the observation that PD-L1 expression is normally clustered in tumour tissues and is co-localized with IFN-γ-producing lymphocytes. Further evidence for this proposal came from a study published by Hu-Lieskovan et al. (43) who found that treatment of patients with B-raf V600E-positive metastatic malignant melanoma with dabrafenib and trametinib significantly increased lymphocyte activation, tumour infiltration and PD-L1 expression.
In this regard Martin et al. (44) provided the first evidence that c-MET-amplified human tumours are susceptible to the expression of PD-L1 by IFN-γ. Using five human cell lines (gastric and lung—all of them with c-MET amplifications or mutations), they also de-menstruated that the PD-L1/PD-L2 induction by IFN-γ could be reversed by a c-MET tyrosine kinase inhibitor (JNJ-38877605) (44) suggesting that c-MET inhibitors can counteract IFN-γ-induced PD-L1 expression. This observation, if confirmed, may add weight to the proposal of the assumed discrepancy of c-MET inhibitors depending on the experimental conditions.
Novel mechanisms of PD-L1 regulation by c-MET
Clearly, there are multiple pathways by which c-MET can influence PD-L1 expression and key player are not fully understood. Amongst them heme oxygenase-1 (HO-1) is of particular interest. HO-1 is a stress-inducible cytoprotective molecule which can by catalysing the degradation of heme into carbon monoxide, biliverdin, ferrous iron (45) promoting cancer growth (46). Using human cell lines Balan and co-workers (47) demonstrated for the first time that PD-L1 overexpression following c-MET activation was associated with increased levels of HO-1, the anti-apoptotic proteins bcl-2 and bcl-xL, and an activation of the ras-raf-pathway. Interestingly, they could also show that knock-down of ras and/or HO-1 resulted in an only minor increase of PD-L1 levels suggesting that the c-MET/ras/HO-1 axis may regulate PD-L1 expression in tumour cells, a finding that might pave the way for the development of HO-1 inhibitors as novel anticancer drugs.
Collectively, to date it is still an open question whether the inhibition of c-MET may or may not favour antitumour immune responses as preclinical evidence is not conclusive and sometimes even contradictory (summarised in Table 1). However, from the clinical per-spective it is still conceivable that cancer patients treated with c-MET inhibitors may benefit from lowering of the adaptive resistance level mediated by PD-L1.
c-MET—prognostic marker
It is now almost two decades ago that somatic c-MET exon 14 mutations have been discovered resulting in increased tumorigenesis and poor clinical outcome (12). Today, more than 70% of lung adenocarcinomas can be defined by driver mutations (e.g., EGFR and K-ras), however, c-MET exon 14 mutations are rare (prevalence 3–4%) and are strongly associated with gene amplification and protein overexpression. Several mutations within the c-MET gene have been discovered so far, and some of them have been identified as resistance mechanisms for recently approved selective c-MET inhibitors (Table 2).

Full table
Of note, although c-MET protein expression was detected in 65% of lung adeno-carcinoma, only 10% of the c-MET-immunohistochemistry positive tumors harbour c-MET gene alterations that triggered protein overexpression suggesting that c-MET per se might not be a suitable biomarker for clinical trials (50).
c-MET mutations and high-level amplification (ratio ≥6) have been found to be almost exclusive to other major driver mutations and define a distinct clinicopathological type of NSCLCs with predominantly sarcomatoid histologies and an aggressive clinical outcome (51).
In the meantime, several researchers have provided compelling evidence that c-MET exon 14 skipping mutations were associated with old age (median age 73 years), the acinar or solid histologic subtype, and high c-MET immunohistochemical expression. Moreover, amongst patients with c-MET exon 14 mutations, 68% were women, and 36% were found to be never-smokers. In addition, tumour burden was found to be low as half of the patients commonly present with stage I disease (52) suggesting that c-MET exon 14 mutation may be an early onset in lung cancer development, and the stepwise addition of c-MET amplification and/or overexpression may contribute to a more aggressive clinical phenotype (52).
However, patients with advanced and/or metastatic NSCLCs were found to have significantly more concurrent c-MET genomic amplification (51). This finding might be of greater importance as older patients tend to have more comorbidities and are less likely to tolerate toxic chemotherapy and, therefore, might be eligible for treatment with TKIs and CPIs with lower site effects. Finally, it should be noted that c-MET exon 14 mutations were found at a higher rate in Asian patients, a finding that has also been reported for EGFR mutations (53).
To date it is generally accepted that c-MET mutations in exon 14 and c-MET amplifications in NSCLCs are clearly associated with dismal survival. Several lines of compelling data from different groups of researchers have added weight to the proposal that c-MET alterations are correlated with worst clinical outcome and a poorer prognosis. Amongst these publications three meta-analyses (54-56) impressively highlighted the role of c-MET in NSCLC patients. The results are shown in Table 3.
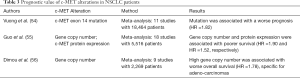
Full table
Collectively, amplification of the c-MET gene, c-MET exon 14 skipping mutations, and overexpression of the c-MET protein are independent marker for worst prognosis and poor clinical outcome in NSCLC patients.
c-MET—detection of amplifications and mutations
c-MET alterations represent an established biomarker to identify patients who might benefit from treatment with c-MET inhibitors (57) however, to date no standardised method for the detection of these alterations has been established. Common technologies comprise fluorescence in situ hybridization (FISH), single-nucleotide polymorphism (SNP) genotyping, quantitative polymerase chain reaction (qPCR), or immunohistochemistry (ICH). In terms of c-MET protein levels it should be noted that detection is dependent on the antibodies used as they have different epitopes and domains.
Based on these caveats a tumour re-biopsy is regarded to be the best alternative, however, this procedure is often not possible and therefore sheds light on the proposal that liquid biopsy techniques [e.g., circulating tumour cells (CTCs) and circulating free DNA (cfDNA)] to address the c-MET status could be the method of choice (58).
In an attempt to further evaluate the utility of a liquid biopsy-based strategy to assess c-MET alterations in cancer patients, Mondelo-Macía et al. (59) investigated the c-MET gene copy number (GCN) status in cfDNA and the c-MET expression in CTCs of 174 cancer patients. In addition, a commercially available droplet digital PCR (ddPCR) technique was employed to detect c-MET amplifications in blood samples from tumour patients. The authors found that c-MET amplification positivity detected by ddPCR was comparable to that detected by FISH. In addition, a comparison with 49 healthy controls the accuracy of the ddPCR technique to detect c-MET amplifications was demonstrated, and a significant correlation between cfDNA concentration and GCN was found. Although a direct comparison of c-MET GCN between plasma and tissue was not done, the authors concluded that c-MET analysis in plasma samples is a validated and robust tool to guide therapies with c-MET inhibitors.
More evidence for this conclusion has been provided by Zhang et al. (60) who also demonstrated that c-MET amplification can be readily detected in the peripheral blood using the ddPCR methodology. In addition, Ikeda and co-workers (61) provided additional evidence that c-MET point mutations can also be detected in liquid biopsies using the digital sequencing of cfDNA of 438 cancer patients (61). In their study they showed that c-MET alterations occurred in 7.1% of patients analysed and was associated with a shorter time to metastasis/recurrence and a poorer survival. Interestingly, a high number of co-altered genes were found in this study which adds weight to the proposal that c-MET inhibitors should be combined with other targeted therapies to optimise the treatment outcome (61).
Taken together these results clear demonstrate that the assessment of the c-MET status (e.g., amplification, mutations) in tumour patients by liquid biopsies is a reliable technique and most likely the method of choice for patients with later treatment lines who are no longer eligible for a second biopsy.
c-MET—efficacy of inhibitors in NSCLC
Most recently two highly selective oral c-MET inhibitors (i.e., capmatinib and tepotinib) have been approved for treatment of NSCLCs harbouring c-MET exon 14 skipping mutations (62,63). Both of these phase II trials demonstrated high ORRs in the first-line setting (48–68%), and an ORR of 41% was reported for capmatinib even in later treatment lines (62) (Table 4). Of note, the GEOMETRY mono-1 trial also demonstrated a high activity in patients with brain metastases (7/13 patients including 4 patients with a complete remission) suggesting that capmatinib may cross readily the blood-brain-barrier (62). This is an important finding that clearly warrants further confirmation in larger clinical trials as brain metastases are often found to be critical for the quality of life and the remaining life span.
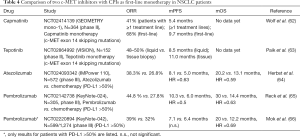
Full table
When compared with other TKIs approved for treatment of NSCLC patients harbouring driver mutations (e.g., EGFR, ROS1, ALK etc.), the results presented for capmatinib and tepotinib are comparable with those reported for these targeted therapies, and even a higher mPFS was found in subsequent treatment lines for capmatinib (62).
As mentioned earlier, based on the current experimental data the interface between c-MET alteration and response to CPI treatment is still controversial and far from being clear. Given the observation that PD-L1 expression is significantly higher in NSCLCs harbouring c-MET alterations, it is interesting to note that ORR and mPFS values for CPIs (e.g., pembrolizumab, atezolizumab) in first-line settings (PD-L1 >50%) appear to be somewhat lower compared with those reported for the novel c-MET inhibitors (Table 4) suggesting that off-target resistance mechanisms may also contribute to this observation.
In this regard two studies attempted to analyse the efficacy of CPI treatment of NSCLC patients harbouring c-MET exon 14 skipping mutations (21,67). Sabari and co-workers analysed 24 NSCLC patients with c-MET exon 14 skipping mutations who received immunotherapy (22 patients with anti-PD-1 or anti-PD-L1 monotherapy, 2 patients received combination therapy of anti-PD-1 and anti-CTLA-4). First-line treatment was given in 11 patients, and 6 and 7 patients were treated with second- and third-line protocols, respectively (24). Amongst these patients the ORR was found to be only 17%; the mPFS was 1.9 months, and OS was 18.9 months. Interestingly, the observed efficacy was neither associated with high PD-L1 levels (2/11 patients) nor with higher TMB (0/8 patients).
In an additional study the same group of researchers (67) retrospectively analysed 551 NSCLC patients with oncogenic driver mutations in terms of their response to CPIs. The vast majority of patients had received PD-1 inhibitors [e.g., nivolumab (N=466) and pembroizumab (N=48)]) whereas the remaining 6% of patients were treated with atezolizumab (N=19) or durvalumab (N=11). Amongst all patients analysed, 36 patients had c-MET exon 14 skipping mutations (6.5%) and 11/36 of these patients revealed a higher PD-L1 expression level when compared with the overall population (30% vs. 10%). For all c-MET patients mPFS was 3.4 months, however, long-term responders were more frequently seen in the c-MET group (23.4%) when compared with other subgroups (e.g., 6.4% for EGFRmut) (56). OS was found to be 18.4 months and was not correlated with PD-L1 expression or number of prior therapies. Of note, mPFS in the c-MET subgroup was also not associated with c-MET exon 14 skipping mutations or other c-MET alterations (67).
Collectively, both studies added weight to the proposal that response to immunotherapy might be impaired in NSCLC patients harbouring c-MET alterations resulting in lower ORRs and shorter mPFS in this molecular subgroup of patients regardless of the PD-L1 expression. Despite the limitation of being retrospective studies these trials provide further evidence that NSCLC patients with druggable oncogenic driver mutations should receive targeted therapy and chemotherapy first before immunotherapy is considered—a finding that has also been noted for other oncogenic driver mutations such as pembrolizumab in EGFRmut patients (68) or durvalumab in ALK/EGFRmut NSCLCs (69), and should be taken into account when conducting future randomised clinical trials.
Efficacy data from prospective randomised clinical trials of CPI treatments in NSCLC patients with c-MET exon 14 mutations, however, are not available so far, but would shed additional light on the optimal utilization of CPIs and c-MET inhibitors in clinical settings.
Future directions: is c-MET an accomplice of EGFR mutations as well?
c-MET amplification and EGFR mutations
Amplification of c-MET is known to be an oncogenic driver (15). The basic mechanism by which c-MET amplification causes EGFR-TKI resistance is associated with the activation of EGFR-independent phosphorylation of ErbB3 and downstream activation of the PI3K/AKT pathway, providing a bypass signaling pathway even in the presence of an EGFR-TKI (70) suggesting that co-targeting both, EGFR and c-MET is required to overcome resistance to EGFR-TKIs due to c-MET amplification.
The c-MET amplification in NSCLCs was found to be only 2–5%. However, the incidence of c-MET amplification was higher in NSCLC patients treated with erlotinib or gefitinib, ranging from 5% to 22% (15). Several lines of evidence, however, suggest that c-MET gene amplification is another important mechanism for TKI resistance in NSCLCs and is detectable in approximately 5–22% of NSCLC patients with acquired resistance to first-generation EGFR-TKIs [reviewed by (71)].
c-MET amplification is a potential resistance pattern of EGFR-TKIs in NSCLC, accounting for 50–60% of the first- and second-generation EGFR-TKIs acquired resistance (70,72) and for 15–19% of the third-generation EGFR-TKIs acquired resistance (72,73). The results clearly demonstrated that c-MET amplification is the most common acquired resistance mechanism to first-line EGFR TKI treatment in NSCLC.
Interestingly, although c-MET amplification can occur with the EGFR T790M mutation, about 60% of c-MET amplification is found without a T790M mutation. Obviously, there is an inverse correlation between the presence of T790M and c-MET gene copy number suggesting a complementary or independent role of the two mechanisms in the acquisition of resistance (74). Similar observations have been made in studies with other third-generation EGFR-TKIs.
Piotrowska et al. (75) analysed tissue biopsies from 32 osimertinib-resistant EGFRmut NSCLC patients and detected 22% of patients carrying c-MET amplification and 19% of patients with an acquired EGFR C797S mutation. Another study by Oxnard et al. (76) documented that among 41 patients who developed resistance to osimertinib and underwent biopsy after relapse, four cases (10%) with c-MET amplification were detected. Analysis of plasma samples from 73 patients with resistance to osimertinib second-line treatment in the large phase III clinical study AURA3 showed that c-MET amplification was the most common (19%) resistance mechanism, followed by EGFR C797X secondary mutation (15%), with ten cases of C797S and one case of C797G (73).
Preclinical data
Some preclinical studies have provided further evidence that inhibition of c-MET with either gene knockdown or a small molecule c-MET inhibitor (crizotinib) combined with osimertinib very effectively inhibited the growth of HCC827/ER and HCC827/AR cells in vitro and in vivo, both harbouring c-MET amplifications (77). This group of researchers also demonstrated that ErbB3 phosphorylation in both, HCC827/ER and HCC827/AR cell lines was minimally inhibited by osimertinib alone, but could be fully suppressed when combined with a c-MET inhibitor both, in vitro and in vivo. This was also seen for phosphorylation of other proteins including AKT, S6, and ERK1/2 suggesting that a full suppression of ErbB3 phosphorylation is tightly associated with the enhanced efficacy of osimertinib and its combination with c-MET inhibition against the growth of EGFR-TKI-resistant cell lines with c-MET amplification (15). Similar results have also been provided by other researchers using different resistant models with c-MET amplification (78,79) which added weight to the proposal that c-MET gene amplification and protein hyperactivation are likely a common resistance mechanism to both first- and third-generation EGFR-TKIs.
Collectively, NSCLCs with c-MET amplification, protein overexpression, or hyper-activation are unlikely to respond to osimertinib or other third-generation EGFR TKIs and based on these findings a similar attempt has been made in the clinic.
Clinical data
It is generally accepted that patients with c-MET amplifications after osimertinib resistance tend to have an inferior mPFS and mOS than patients without the appearance of or increase in c-MET amplification (80). Therefore, effective strategies for the treatment of patients with c-MET-amplified NSCLCs who have relapsed from first- or second-generation EGFR-TKI treatment, or patients who develop acquired resistance to osimertinib or other third-generation TKIs due to c-MET amplification and/or protein hyperactivation are urgently needed.
When c-MET inhibitors are combined with TKIs in the upstream or downstream signaling pathways, they can inhibit parallel kinase signaling from other receptors which may improve the clinical outcomes. Recently, Piotrowska and co-workers (75) provided the first evidence that tumour heterogeneity and co-existence of T790M and T790M wild-type resistant subclones drive the mixed response to third-generation EGFRmut inhibitors in NSCLCs. Similar observations have been detailed in studies with other third-generation TKIs which added weight to the proposal that monotherapy with osimertinib (or other third-generation TKIs) will be ineffective in NSCLC patients harbouring c-MET amplifications suggesting that concomitant inhibition of both, EGFRmut and c-MET is required to overcome resistance to EGFRmut-targeting TKIs in NSCLCs.
Based on these preclinical findings Wu et al. (81) reported results from a phase Ib/II study with capmatinib and gefitinib in NSCLC patients with acquired resistance to gefitinib, erlotinib, or afatinib and c-MET amplifications (gene copy number ≥6). Overall, 61 patients were treated in phase IB, and 100 patients were treated in phase II. In the phase IB part ORR was 23% across all doses and was regardless of the c-MET status. Increased activity, however, was observed in patients with a high c-MET copy number, with a phase II ORR of 47%. The most common drug-related adverse events were nausea (28%), peripheral edema (22%), decreased appetite (21%), and rash (20%). In contrast to a number of other combination studies, the combination of capmatinib and gefitinib was found to be tolerable. From this study the authors concluded that capmatinib in combination with an EGFRmut TKI can restore sensitivity in TKI-resistant NSCLC patients harbouring EGFR mutations.
Similar results have been reported by Cheng et al. (82) who could also demonstrate that the c-MET inhibitor tepotinib restored sensitivity to gefitinib in EGFRmut NSCLC patients with acquired resistance to first-generation TKIs and c-MET amplifications when compared with chemotherapy. Among patients with c-MET protein overexpression, the response rate of the combination was 68.4% vs. 33.3% in the chemotherapy group. Subgroup analysis revealed that patients with c-MET gene amplification receiving tepotinib plus gefitinib had a mPFS of 21.2 months, much longer than that for chemotherapy (4.2 months). Again, the combination treatment was well tolerated (82).
Although the results from the AURA3 and the FLAURA trials led to the approval of osimertinib (a third-generation TKI with activity in NSCLCs harbouring the T790M mutation as first- and second-line treatment), it should be noted that 20% of these patients did not respond to osimertinib. In one third of this resistant population the osimertinib resistance could be linked to the novel C797S mutation, whereas in many other cases c-MET amplifications as a resistance bypass mechanism causing EGFRmut-TKI resistance have been identified suggesting that a combination of a c-MET and a EGFRmut inhibitor may be of benefit to overcome the observed resistance in these NSCLC patients. The current treatment algorithm for NSCLC patients harbouring EGFR mutations is shown in Figure 1.

Conclusions
Although several experimental studies have provided significant evidence that a relationship between c-MET alterations (mutations, amplifications) and the immune response exits, the underlying mechanisms are not conclusive but multifactorial and are far from being clear. c-MET alterations have been found to be positively correlated with enhanced expression of immune-inhibitory molecules (e.g., PD-L1) and decreased expression of co-stimulatory markers (e.g., CD137, CD252 etc.), and c-MET obviously is implicated in controlling the inflamed TME. In addition, c-MET amplification has been found to be a major mechanism for TKIs targeting EGFR mutations in NSCLCs which will provide the basis for combining EGFRmut TKIs and c-MET inhibitors in the clinic. The clinical efficacy of CPIs in NSCLC patients harbouring c-MET alterations, however, is not yet established and further research will certainly provide some guidance as to optimally utilise CPS and c-MET inhibitors in the future.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at http://dx.doi.org/10.21037/tlcr-21-124
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tlcr-21-124). Both authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Arbour KC, Riely GJ. Systemic therapy for locally advanced and metastatic non-small cell lung cancer: a review. JAMA 2019;322:764-74. [Crossref] [PubMed]
- Dempke WCM. Targeted therapy for NSCLC—a double-edged sword? Anticancer Res 2015;35:2503-12. [PubMed]
- Dempke WCM, Sellmann L, Fenchel K, et al. Immunotherapies for NSCLC: are we cutting the gordian helix? Anticancer Res 2015;35:5745-57. [PubMed]
- Dempke WCM, Fenchel K, Dale SP. Programmed cell death ligand-1 (PD-L1) as a biomarker for non-small cell lung cancer (NSCLC) treatment—are we barking up the wrong tree? Transl Lung Cancer Res 2018;7:S275-9. [Crossref] [PubMed]
- Huang X, Li E, Shen H, et al. Targeting the HGF/MET axis in cancer therapy: challenges in resistance and opportunities for improvement. Front Cell Dev Biol 2020;8:152 [Crossref] [PubMed]
- Hartmann S, Bhola NE, Grandis JR. HGF/Met signaling in head and neck cancer: impact on the tumor microenvironment. Clin Cancer Res 2016;22:4005-13. [Crossref] [PubMed]
- Zhen Z, Giordano S, Longati P, et al. Structural and functional domains critical for con-stitutive activation of the HGF-receptor (Met). Oncogene 1994;9:1691-7. [PubMed]
- Zhu H, Naujokas MA, Fixman ED, et al. Tyrosine 1356 in the carboxyl-terminal tail of the HGF/SF receptor is essential for the transduction of signals for cell motility and morphogenesis. J Biol Chem 1994;269:29943-8. [Crossref] [PubMed]
- Ferracini R, Longati P, Naldini L, et al. Identification of the major autophosphorylation site of the Met/hepatocyte growth factor receptor tyrosine kinase. J Biol Chem 1991;266:19558-64. [Crossref] [PubMed]
- Dempke WCM, Uciechowski P, Fenchel K, et al. Targeting SHP-1,2 and SHIP pathways—a novel strategy for cancer treatment? Oncology 2018;95:257-69. [Crossref] [PubMed]
- Ma PC. MET receptor juxtamembrane exon 14 alternative splice variant: novel cancer genomic predictive biomarker. Cancer Discov 2015;5:802-5. [Crossref] [PubMed]
- Kong-Beltran M, Seshagiri S, Zha J, et al. Somatic mutations lead to an oncogenic deletion of Met in lung cancer. Cancer Res 2006;66:283-9. [Crossref] [PubMed]
- Gherardi E, Birchmeier W, Birchmeier C, et al. Targeting MET in cancer: rationale and progress. Nat Rev Cancer 2012;12:89-103. [Crossref] [PubMed]
- Frampton GM, Ali SM, Rosenzweig M, et al. Activation of MET via diverse exon 14 splicing alterations occcurs in multiple tumor types and confers clinical sensitivity to MET inhibitors. Cancer Discov 2015;5:850-9. [Crossref] [PubMed]
- Liang H, Wang M. MET oncogene in non-small cell lung cancer: mechanism of MET dysregulation and agents targeting the HGF/c-MET axis. Onco Targets Ther 2020;13:2491-510. [Crossref] [PubMed]
- Lan B, Ma C, Zhang C, et al. Association between PD-L1 expression and driver gene status in non-small-cell lung cancer: a meta-analysis. Oncotarget 2018;9:7684-99. [Crossref] [PubMed]
- Albitar M, Sudarsanam S, Ma W, et al. Correlation of MET gene amplification and TP53 mutation with PD-L1 expression in non-small cell lung cancer. Oncotarget 2018;9:13682-93. [Crossref] [PubMed]
- Schoenfeld AJ, Rizvi H, Bandlamudi C, et al. Clinical and molecular correlates of PD-L1 expression in patients with lung adenocarcinomas. Ann Oncol 2020;31:599-608. [Crossref] [PubMed]
- Saigi M, Alburgquerque-Bejar JJ, Leer-Florin A, et al. MET-oncogenic and JAK2-inactivating alterations are independent factors that affect regulation of PD-L1 expression in lung cancer. Clin Cancer Res 2018;24:4579-87. [Crossref] [PubMed]
- Zhang Y, Wang L, Li Y, et al. Protein expression of programmed death 1 ligand and ligand 2 independently predict poor prognosis in surgically resected lung adenocarcinoma. Onco Targets Ther 2014;7:567-73. [Crossref] [PubMed]
- Xu Z, Li H, Dong Y, et al. Incidence and PD-L1 expression of MET 14 skipping in Chinese population: a non-selective NSCLC cohort study using RNA-based sequencing. Onco Targets Ther 2020;13:6245-53. [Crossref] [PubMed]
- Suzawa K, Offin M, Lu D, et al. Activation of KRAS mediates resistance to targeted therapy in MET exon-14-mutant non-small cell lung cancer. Clin Cancer Res 2019;25:1248-60. [Crossref] [PubMed]
- Yoshimura K, Inoue Y, Tsuchiya K, et al. Elucidation of the relationships of MET protein expression and gene copy number status with PD-L1 expression and the immune microenvironment in non-small cell lung cancer. Lung Cancer 2020;141:21-31. [Crossref] [PubMed]
- Sabari JK, Leonardi GC, Shu CA, et al. PD-L1 expression, tumor mutational burden, and response to immunotherapy in patients with MET exon 14 altered lung cancers. Ann Oncol 2018;29:2085-91. [Crossref] [PubMed]
- Belli C, Trapani D, Viale G, et al. Targeting the microenvironment in solid tumors. Cancer Treat Rev 2018;65:22-32. [Crossref] [PubMed]
- Chen Y, Song Y, Du W, et al. Tumor-associated macrophages: an accomplice in solid tumor progression. J Biomed Sci 2019;26:78-87. [Crossref] [PubMed]
- Knowles LM, Stabile LP, Egloff AM, et al. HGC and c-MET participate in paracrine tumorigenic pathways in head and neck squamous cell cancer. Clin Cancer Res 2009;15:3740-50. [Crossref] [PubMed]
- Rutella S, Bonanno G, Procoli A, et al. Hepatocyte growth factor favors monocyte differentiation into regulatory interleukin (IL)-10++IL-12low/neg accessory cells with dendritic-cell features. Blood 2006;108:218-27. [Crossref] [PubMed]
- Benkhoucha M, Santiago-Raber ML, Schneiter G, et al. Hepatocyte growth factor inhibits CNS autoimmunity by inducing tolerogenic dendritic cells and CD25+FoxP3+ regulatory T cells. Proc Natl Acad Sci USA 2010;107:6424-9. [Crossref] [PubMed]
- Glodde N, Bald T, van der Boorn-Konijnenberg D, et al. Reactive neutrophil responses dependent on the receptor tyrosine kinase c-MET limit cancer immunotherapy. Immunity 2017;47:789-802.e9. [Crossref] [PubMed]
- Voehringer D, Koschella M, Pircher H. Lack of proliferative capacity of human effector and memory T cells expressing killer cell lectin-like receptor G1 (KLRG1). Blood 2002;100:3698-702. [Crossref] [PubMed]
- Li H, Li CW, Li X, et al. MET inhibitors promote liver tumor evasion of the immune response by stabilizing PDL1. Gastroenterology 2019;156:1849-61.e13. [Crossref] [PubMed]
- Dimou A, Syrigos KN. The role of GSK3β in T lymphocytes in the tumor microenvironment. Front Oncol 2020;10:1221-8. [Crossref] [PubMed]
- Dempke WCM, Fenchel K, Uciechowski P, et al. Targeting developmental pathways—the Achilles heel of cancer? Oncology 2017;93:213-23. [Crossref] [PubMed]
- Gros A, Robbins PF, Yao X, et al. PD-1 indentifies the patient-specific CD8(+) tumor-reactive repertoire infiltrating human tumors. J Clin Invest 2014;124:2246-59. [Crossref] [PubMed]
- Ohteki T, Parsons M, Zakarian A, et al. Negative regulation of T cell proliferation and interleukin 2 production by the serine-threonine kinase GSK-3. J Exp Med 2000;192:99-104. [Crossref] [PubMed]
- Li CW, Lim SO, Xia W, et al. Glycosylation and stabilization of programmed death ligand-1 suppressed T-cell activity. Nat Commun 2016;7:12632-43. [Crossref] [PubMed]
- Parsa AT, Waldron JS, Panner A, et al. Loss of tumor suppressor PTEN function increases B7-H1 expression and immunoresistance in glioma. Nat Med 2007;13:84-8. [Crossref] [PubMed]
- Sun X, Li CW, Wang WJ, et al. Inhibition of c-MET upregulates PD-L1 expression in lung adenocarcinoma. Am J Cancer Res 2020;10:564-71. [PubMed]
- Ahn HK, Kim S, Kwon D, et al. MET receptor tyrosine kinase regulates the expression of co-stimulatory and co-inhibitory molecules in tumor cells and contributes to PD-L1-mediated suppression of immune cell function. Int J Mol Sci 2019;20:4287-4304. [Crossref] [PubMed]
- Reis H, Metzenbacher M, Goetz M, et al. MET expression in advanced non-small-cell lung cancer: effect on clinical outcomes of chemotherapy, targeted therapy, and immuno-therapy. Clin Lung Cancer 2018;19:e441-63. [Crossref] [PubMed]
- Garcia-Diaz A, Shen DS, Moreno BH, et al. Interferon receptor signaling pathways regulating PD-L1 and PD-L2 expression. Cell Rep 2017;19:1189-201. [Crossref] [PubMed]
- Hu-Lieskovan S, Mok S, Moreno BL, et al. Improved antitumor activity of immunotherapy with BRAF and MEK inhibitors in BRAFV600E melanoma. Sci Transl Med 2015;7:279ra41 [Crossref] [PubMed]
- Martin V, Chiriaco C, Modica C, et al. Met inhibition revokes IFNγ-induction of PD-1 ligands in MET-amplified tumours. Brit J Cancer 2019;120:527-36. [Crossref] [PubMed]
- Agarwal A, Nick HS. Renal response to tissue injury: lessons from heme oxygenase-1 gene ablation and expression. J Am Soc Nephrol 2000;11:965-73. [Crossref] [PubMed]
- Was H, Dulak J, Jozkowicz A. Heme oxygenase-1 in tumor biology and therapy. Curr Drug Targets 2010;11:1551-70. [Crossref] [PubMed]
- Balan M, Teran EMY, Waaga-Gasser AM, et al. Novel roles of c-MET in the survival of renal cancer cells through the regulation of HO-1 and PD-L1 expression. J Biol Chem 2015;290:8110-20. [Crossref] [PubMed]
- Fujino T, Kobayashi Y, Suka K, et al. Sensitivity and resistance of MET exon 14 mutations in lung cancer to eight MET tyrosine kinase inhibitors in vitro. J Thorac Oncol 2019;14:1753-65. [Crossref] [PubMed]
- Ji F, Liu X, Wu Y, et al. Overexpression of PI3K p110alpha contributes to acquired resistance to MET inhibitor, in MET-amplified SNU-5 gastric xenografts. Drug Des Devel Ther 2015;9:5697-704. [PubMed]
- Yeung SF, Tong JHM, Law PPW, et al. Profiling of oncogenic driver events in lung adenocarcinoma revealed MET mutation as independent prognostic factor. J Thorac Oncol 2015;10:1292-300. [Crossref] [PubMed]
- Tong JH, Yeung SF, Chan AWH, et al. MET amplification and exon 14 splice site mutation define unique molecular subgroups of non-small cell lung carcinoma with poor prognosis. Clin Cancer Res 2016;22:3048-56. [Crossref] [PubMed]
- Awad MM, Oxnard GR, Jackman DM, et al. MET exon 14 mutations in non-small-cell lung cancer are associated with advanced age and stage-dependent MET genomic amplification and c-MET overexpression. J Clin Oncol 2016;34:721-30. [Crossref] [PubMed]
- Lee GD, Lee SE, Oh DY, et al. MET exon 14 skipping mutations in lung adenocarcinoma: clinicopathologic implications and prognostic values. J Thorac Oncol 2017;12:1233-46. [Crossref] [PubMed]
- Vuong HG, No ATN, Altibi AMA, et al. Clinicopathological implications of MET exon 14 mutations in non-small cell lung cancer—a systematic review and meta-analysis. Lung Cancer 2018;123:76-82. [Crossref] [PubMed]
- Guo B, Cen H, Tan X, et al. Prognostic value of MET gene copy number and protein expression in patients with surgically resected non-small cell lung cancer: a meta-analysis of published literatures. PLoS One 2014;9:e99399 [Crossref] [PubMed]
- Dimou A, Non L, Chae YK, et al. MET gene copy number predicts worse overall survival in patients with non-small cell lung cancer (NSCLC); a systematic review and meta-analysis. PLoS One 2014;9:e107677 [Crossref] [PubMed]
- Zhang Y, Du Z, Zhang M. Biomarker development in MET-targeted therapy. Oncotarget 2016;7:37370-89. [Crossref] [PubMed]
- Ilie M, Hofman V, Long E, et al. Current challenges for detection of circulating tumor cells and cell-free circulating nucleic acids, and their characterization in non-small cell lung cancinoma patients. What is the best blood substrate for personalized medicine? Ann Transl Med 2014;2:107-17. [PubMed]
- Mondelo-Macía P, Rodríguez-López C, Valiña L, et al. Detection of MET alterations using cell free DNA and circulating tumor cells from cancer patients. Cells 2020;9:522. [Crossref] [PubMed]
- Zhang Y, Tang ET, Du Z. Detection of MET gene copy number in cancer samples using the droplet digital PCR method. PLoS One 2016;11:e0146784 [Crossref] [PubMed]
- Ikeda S, Schwaederle M, Mohindra M, et al. MET alterations detected in blood-derived circulating tumor DNA correlate with bone metastases and poor prognosis. J Hematol Oncol 2018;11:76-95. [Crossref] [PubMed]
- Wolf J, Seto T, Han JY, et al. Capmatinib in MET exon 14-mutated or MET-amplified non-small-cell lung cancer. N Engl J Med 2020;383:944-57. [Crossref] [PubMed]
- Paik PK, Felip E, Veillon R, et al. Tepotinib in non-small-cell lung cancer with MET exon 14 skipping mutations. N Engl J Med 2020;383:931-43. [Crossref] [PubMed]
- Herbst RS, Giaccone G, de Marinis F, et al. Atezolizumab for first-line treatment of PD-l1-selected patients with NSCLC. N Engl J Med 2020;383:1328-39. [Crossref] [PubMed]
- Reck M, Rodriguez-Abreu D, Robinson AG, et al. Pembrolizumab vs. chemotherapy for PD-L1-positive non-small-cell lung cancer. N Engl J Med 2016;375:1823-33. [Crossref] [PubMed]
- Mok TSK, Wu YL, Kudaba I, et al. Pembrolizumab vs. chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): a randomised, open-label, controlled, phase 3 trial. Lancet 2019;393:1819-30. [Crossref] [PubMed]
- Mazieres J, Drilon A, Lusque A, et al. Immune checkpoint inhibitors for patients with advanced lung cancer and oncogenic driver alterations: results from the IMMUNOTARGET registry. Ann Oncol 2019;30:1321-8. [Crossref] [PubMed]
- Lisberg A, Cummings A, Goldman JW, et al. A phase II study of pembrolizumab in EGFR-mutant, PD-L1+, tyrosine kinase naïve patients with advanced NSCLC. J Thorac Oncol 2018;13:1138-45. [Crossref] [PubMed]
- Garassino MC, Cho BC, Kim JH, et al. Durvalumab as third-line or later treatment for advanced non-small-cell lung cancer (ATLANTIC): an open-label, single-arm, phase 2 study. Lancet Oncol 2018;19:521-36. [Crossref] [PubMed]
- Engelman JA, Zejnullahu K, Mitsudomi T, et al. MET amplification leads to gefitinib resistance in lung cancer by activating ERBB3 signaling. Science 2007;316:1039-43. [Crossref] [PubMed]
- Wang Q, Yang S, Wang K, et al. MET inhibitors for targeted therapy of EGFR TKI-resistant lung cancer. J Hematol Oncol 2019;12:63-74. [Crossref] [PubMed]
- Ramalingam SS, Cheng Y, Zhou C, et al. Mechanisms of acquired resistance to first-line osimertinib: preliminary data from the phase III FLAURA study. Ann Oncol 2018;29:740. [Crossref]
- Papadimitrakopoulou VA, Wu YL, Han JY, et al. Analysis of resistance mechnisms to osimertinib in patients with EGFR T790M advanced NSCLC from the AURA3 study. Ann Oncol 2018;29:741-8. [Crossref]
- Suda K, Murakami I, Katayama T, et al. Reciprocal and complementary role of MET amplification and EGFR T790M mutation in acquired resistance to kinase inhibitors in lung cancer. Clin Cancer Res 2010;16:5489-98. [Crossref] [PubMed]
- Piotrowska Z, Isozaki H, Lennerz JK, et al. Landscape of acquired resistance to osimertinib in EGFR-mutant NSCLC and clinical validation of combined EGFR and RET inhibition with osimertinib and BLU-667 for acquired RET fusion. Cancer Discov 2018;8:1529-39. [Crossref] [PubMed]
- Oxnard GR, Hu Y, Mileham KF, et al. Assessment of resistance mechanisms and clinical implications in patients with EGFR T790M-positive lung cancer and acquired resistance to osimertinib. JAMA Oncol 2018;4:1527-34. [Crossref] [PubMed]
- Shi P, Oh YT, Zhang G, et al. Met gene amplification and protein hyperactivation is a mechanism of resistance to both first and third generation EGFR inhibition in lung cancer treatment. Cancer Lett 2016;380:494-504. [Crossref] [PubMed]
- Ninomiya K, Ohashi K, Makimoto G, et al. MET or NRAS amplification is an acquired resistance mechanism to the third-generation EGFR inhibitor naquotinib. Sci Rep 2018;8:1955. [Crossref] [PubMed]
- Xu W, Tang W, Li T, et al. Overcoming resistance to AC0010, a third generation of EGFR inhibitor, by targeting c-MET and BCL-2. Neoplasia 2019;21:41-51. [Crossref] [PubMed]
- Wang Y, Li L, Han R, et al. Clinical analysis by next-generation sequencing for NSCLC patients with MET amplification resistant to osimertinib. Lung Cancer 2018;118:105-10. [Crossref] [PubMed]
- Wu YL, Zhang L, Kim DW, et al. Phase Ib/II study of capmatinib (INC280) plus gefitinib after failure of epidermal growth factor receptor (EGFR) inhibitor therapy in patients with EGFR-mutant, MET factor-dysregulated non-small-cell lung cancer. J Clin Oncol 2018;36:3101-09. [Crossref] [PubMed]
- Cheng Y, Zhou J, Lu S, et al. Phase II study of tepotinib + gefitinib (TEP + GEF) in MET-positive (MET+)/epidermal growth factor receptor (EGFR)-mutant (MT) non-small cell lung cancer (NSCLC). Ann Oncol 2018;29:493. [Crossref]
- Wang S, Song Y, Liu D. EA1045: the fourth-generation EGFR inhibitor overcoming T790M and C797S resistance. Cancer Lett 2017;385:51-4. [Crossref] [PubMed]


