
PD-L1 expression in pulmonary lymphoepithelioma-like carcinoma: is it a prognostic biomarker?
With great interest, we read the article entitled “The clinicopathological and prognostic significance of PD-L1 expression assessed by immunohistochemistry in lung cancer: a meta-analysis of 50 studies with 11,383 patients” by Li and colleagues in Translational Lung Cancer Research (1). They presented a comprehensive and comparable analysis based on data from 50 studies, and demonstrated that high programmed death-ligand 1 (PD-L1) expression was negatively correlated with overall survival (OS) for patients with lung cancer, especially in non-small cell lung carcinoma (NSCLC), adenocarcinoma (ADC), squamous cell carcinoma (SCC), lymphoepithelioma-like carcinoma (LELC). Due to their findings might have an impact on current clinical practice, several questions deserve attention.
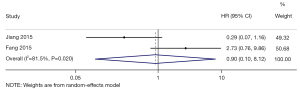
Firstly, the authors made several mistakes in extracting hazard ratios (HRs) and 95% confident intervals (95% CIs) from two studies on LELC (2,3). Fang et al. (2) showed that patients with high PD-L1 expression were prone to inferior OS (HR: 2.730, 95% CI: 0.756–9.863). Unfortunately, Li et al. didn’t find that they had mistaken 9.86 for 9.81. Besides, the authors forgot to convert HR and 95% CI in another included article by Jiang et al. (3). Jiang’s study revealed that a HR and 95% CI of low/high PD-L1 expression for OS was 3.436 and 0.863–13.684. The HR represents the relative difference between only two groups, and has been defined as the ratio of (risk of outcome in one group)/(risk of outcome in another group), occurring at a given interval of time (4). The result of the calculation depends on whether the investigator chooses to calculate the ratio of hazards for (Group A)/(Group B) or to calculate the ratio of hazards for (Group B)/(Group A) (5,6). According to the data extraction of this meta-analysis, the HR of this research was adopted in the opposite direction. Thus, a correct value of 0.291 (0.073–1.159) was re-calculated. After reanalysis, the pooled result suggested no significant association of OS with PD-L1 expression in primary pulmonary LELC (pLELC) (HR: 0.90, 95% CI: 0.10–8.12, P=0.93; I2=81.5%, P=0.02; random-effects model) (Figure 1). Then, the misleading conclusions might also be produced in several other analyses involving these two studies.
Secondly, it was shown that the cut-off value for PD-L1 positivity was 5% in Fang’s study (2) in Tab. 2. After reviewing the article from Fang and colleagues, we found that Fang et al. (2) definitely defined cases with more than 5% expression of PD-L1 as positive ones. However, PD-L1 H-score 30 was further determined as the best threshold to discriminate OS; thus they performed the survival analysis based on dividing patients into those with low and high PD-L1 expression (H-score ≤30 and >30, respectively).
Thirdly, in the abstract result, the P values of heterogeneity had been evidently misused as P values for meta-analysis. And the correct ones were not displayed in the text or tables. Moreover, there existed overlap between the populations enrolled in the meta-analysis, as the above two studies (2,3) included patients from the same department (State Key Laboratory of Oncology in South China, Collaborative Innovation Center of Cancer Medicine, Sun Yat-sen University Cancer Center) with an overlapping period (between 2008 and 2012). That contradicted the inclusion criteria that only the most recent or complete study was included when the same patient population existed in more than one study.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was a standard submission to the journal. The article did not undergo external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-22-473/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Li H, Xu Y, Wan B, et al. The clinicopathological and prognostic significance of PD-L1 expression assessed by immunohistochemistry in lung cancer: a meta-analysis of 50 studies with 11,383 patients. Transl Lung Cancer Res 2019;8:429-49. [Crossref] [PubMed]
- Fang W, Hong S, Chen N, et al. PD-L1 is remarkably over-expressed in EBV-associated pulmonary lymphoepithelioma-like carcinoma and related to poor disease-free survival. Oncotarget 2015;6:33019-32. [Crossref] [PubMed]
- Jiang L, Wang L, Li PF, et al. Positive expression of programmed death ligand-1 correlates with superior outcomes and might be a therapeutic target in primary pulmonary lymphoepithelioma-like carcinoma. Onco Targets Ther 2015;8:1451-7. [PubMed]
- Dawson B, Trapp RG. Basic and clinical biostatistics. 4th ed. New York: Lange Medical Books, 2004: 407.
- Machin D, Cheung YB. Survival analysis: a practical approach. 2nd ed. Hoboken: John Wiley & Sons, Inc., 2006: 62.
- Crowley J. Handbook of statistics in clinical oncology. New York: Marcel Dekker, 2001: 541.


