
Implementation of programmed death-ligand 1 (PD-L1) expression as a prognostic biomarker for patients with lung cancer
We thank Li et al. for showing interest in our article entitled “The clinicopathological and prognostic significance of programmed death-ligand 1 (PD-L1) expression assessed by immunohistochemistry in lung cancer: a meta-analysis of 50 studies with 11,383 patients” (1). We would like to respond to the concerns one by one raised by Li et al. (2).
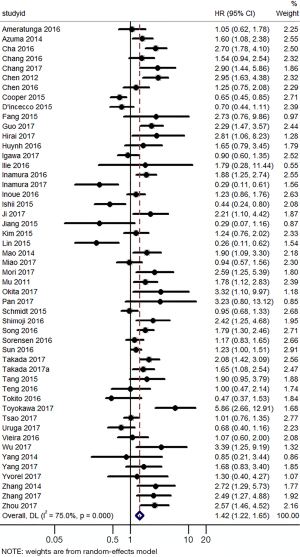
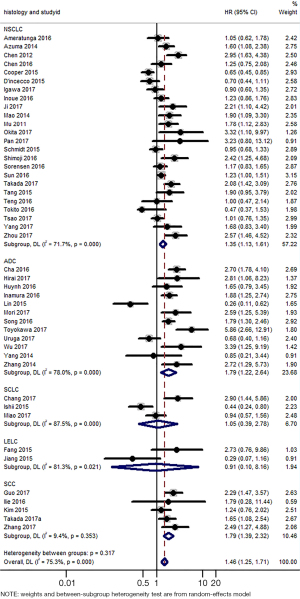
Firstly, we felt sorry for the carelessness in extracting hazard ratios (HRs) and 95% confident intervals (95% CIs) from two studies on lymphoepithelioma-like carcinoma (LELC) (3,4). We thus performed additional analysis with upper limit of 9.863 and converted HR and 95% CI, and the results did not alter the overall findings. After reanalysis, the pooled HRs and 95% CIs suggested that PD-L1 immunohistochemistry (IHC) expression was related to poor OS in lung cancer (HR =1.42, 95% CI: 1.22–1.65) (Figure 1), consistent with results in the primary analysis. Subgroup analyses according to histology (Figure 2) revealed that high PD-L1 expression was significantly related to poor overall survival (OS) of non-small cell lung cancer (NSCLC) patients (HR =1.35, 95% CI: 1.13–1.61), adenocarcinoma (ADC) patients (HR =1.79, 95% CI: 1.22–2.64), squamous cell carcinoma (SCC) patients (HR =1.79, 95% CI: 1.39–2.32), but there was no association of PD-L1 expression with survival in small cell lung cancer (SCLC) patients (HR =1.05, 95% CI: 0.39–2.78) and LELC patients (HR =0.91, 95% CI: 0.10–8.16). In fact, the relationship between PD-L1 expression and prognosis in LELC has long been debated and remains controversial. A recent study by Sha et al. (5) showed that participants with positive PD-L1 expression tended to have longer progression-free survival (PFS) and OS times than those with negative PD-L1 expression, while Yu et al. (6) revealed that positive expression of PD-L1 in tumor cells had no association with OS in LELC. Different testing platforms and thresholds for defining positive PD-L1 expression may partly explained this discrepancy. More studies are needed to explore the prognostic significance of PD-L1 expression in LELC patients.
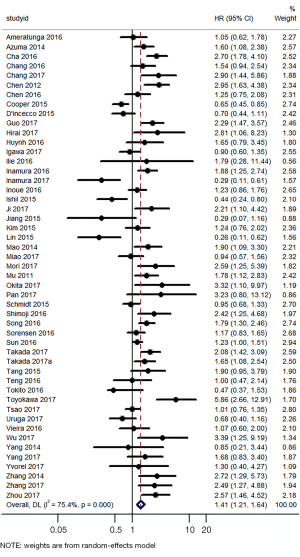
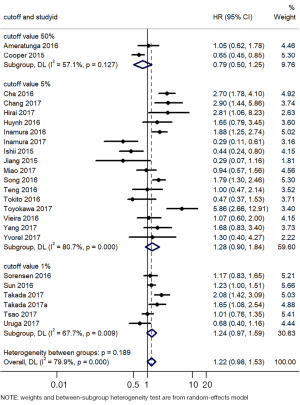
Secondly, Fang and colleagues defined cases with more than 5% expression of PD-L1 as positive ones while PD-L1 H-score 30 was further determined as the best threshold to discriminate OS and analyzed in the Cox proportional hazard regression analysis. The authors did not clearly illustrate the definition of higher or positive PD-L1 expression as previous publications usually divided patients into high/low PD-L1 expression based on PD-L1 expression values (5%, etc.). We re-performed the subgroup analysis based on cutoff value (Figure 3), which was comparable with results in our previous analysis.
Thirdly, we would like to emphasize that P values in the Abstract indeed indicated values of heterogeneity. Although random-effect models were used to deal with significant heterogeneity in both primary and subgroup analyses in the meta-analysis, enough attention should be paid to and the findings need be cautiously interpreted (7).
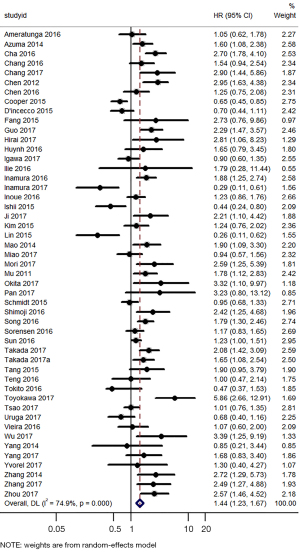
Moreover, we agreed with Li et al. that the above two studies (3,4) may be overlapped. However, the two studies were conducted separately by two research teams. Jiang et al. enrolled 79 pulmonary LELC cases from January 2001 to December 2013 while Fang et al. enrolled 113 surgically resected pulmonary LELC cases from January 2008 to December 2012. In fact, it is hard to conclude whether patients in the two studies were overlapped. We further conducted sensitivity analysis by omitting one study each time and the results remain robust (Figures 4,5).
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Translational Lung Cancer Research. The article did not undergo external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-2022-5/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Li H, Xu Y, Wan B, et al. The clinicopathological and prognostic significance of PD-L1 expression assessed by immunohistochemistry in lung cancer: a meta-analysis of 50 studies with 11,383 patients. Transl Lung Cancer Res 2019;8:429-49. [Crossref] [PubMed]
- Li W, Zhang X, Huang J, et al. PD-L1 expression in pulmonary lymphoepithelioma-like carcinoma: is it a prognostic biomarker? Transl Lung Cancer Res 2022; [Crossref]
- Fang W, Hong S, Chen N, et al. PD-L1 is remarkably over-expressed in EBV-associated pulmonary lymphoepithelioma-like carcinoma and related to poor disease-free survival. Oncotarget 2015;6:33019-32. [Crossref] [PubMed]
- Jiang L, Wang L, Li PF, et al. Positive expression of programmed death ligand-1 correlates with superior outcomes and might be a therapeutic target in primary pulmonary lymphoepithelioma-like carcinoma. Onco Targets Ther 2015;8:1451-7. [PubMed]
- Sha Z, Wei Y, Gao T, et al. Clinical observation of pulmonary lymphoepithelioma-like carcinoma. J Thorac Dis 2021;13:5683-90. [Crossref] [PubMed]
- Yu XY, Zhang XW, Wang F, et al. Correlation and prognostic significance of PD-L1 and P53 expression in resected primary pulmonary lymphoepithelioma-like carcinoma. J Thorac Dis 2018;10:1891-902. [Crossref] [PubMed]
- Lee Y. Fixed-effect versus random-effect models for evaluating therapeutic preferences. Stat Med 2002;21:2325-30. [Crossref] [PubMed]


