
Type 2 diabetes mellitus does not increase the risk of lung cancer among never-smokers: a nationwide cohort study
Introduction
Lung cancer is the most frequently diagnosed cancer and the leading cause of cancer-related death among both male and female populations worldwide (1). Smoking is well known as the major risk factor for lung cancer and other factors such as insulin resistance and type 2 diabetes have reported to be increase lung cancer risk in smokers (2).
Among smoking-unrelated risk factors for lung cancer development, diabetes mellitus is considered an independent risk factor (3). However, contradictory and often conflicting findings have been reported in cohort studies (4).
The Korean National Health Insurance Services (NHIS), as a single-payer health insurance system, covers almost the entire population of South Korea. NHIS also provides biennial health examinations to any individuals aged 40 years and older. Medication exposure of an individual can also be obtained from the NHIS claims database which contains prescription records.
Using this database, this study aimed to evaluate the effect of type 2 diabetes mellitus (T2DM) and abnormal fasting blood sugar (FBS) level on lung cancer incidences within the never-smoker Korean papulations.
Methods
We analyzed NHIS data from a standardized a 12-year longitudinal cohort of health examination to investigate the effects of T2DM and abnormal FBS levels on lung cancer among the nonsmoker population. Figure 1 shows a schematic flow chart of data extraction and inclusion criteria.
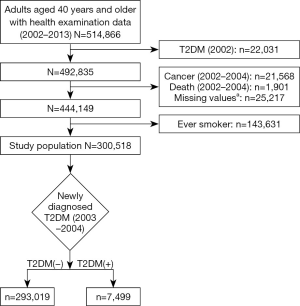
T2DM patient population was identified by anti-diabetic medication prescription, as outlined by the International Classification of Diseases code-10th Revision (ICD-10) pertaining to T2DM (E11-E14). Data from the first year (January 1, 2002 to December 31, 2002) was used to washout diagnosed T2DM patients in order to exclude those who already had T2DM for an unknown period prior to the start date. Any cancer patients and participants who passed away during the first three years (January 1, 2002 to December 31, 2004) were excluded to minimize bias on incidence and death of lung cancer. The never-smoker population was defined as individuals who self-reported to have no experience in smoking. As such, we excluded the ever-smoker populations. T2DM patients defined as those who were newly diagnosed T2DM at the period from January 1, 2003 to December 31, 2004. In addition, the association between fasting blood glucose and lung cancer was also analyzed because of some participants that were not diagnosed with T2DM, but showed abnormal FBS levels.
The cohort entry date was defined as January 1, 2005, and the follow-up observation period was extended to December 31, 2013. Throughout this period, newly diagnosed lung cancer patients were identified to avoid immortal time bias. Lung cancer patients were defined as individuals who visited outpatient ≥2 times, or were hospitalized at least once or passed away with a C34 ICD-10 code. Sociodemographic, medical, and health-related behavior data from 2003 to 2004 (before cohort entry date) were extracted.
Cox proportional hazards regression analysis with T2DM status and FBS status as exposures were employed to estimate hazard ratios (HRs) and 95% confidence interval (CI). FBS status was defined as hypoglycemic (<60 mg/dL), normal (≥60, <100 mg/dL), prediabetic (≥100, <125 mg/dL), and diabetic level (≥126 mg/dL).
Statistical analyses were performed using STATA software version 14.0 (Stata Co., College Station, TX, USA), and P values less than 0.05 were considered statistically significant.
Results
Table 1 shows the baseline characteristics of study population separated by T2DM status within the never-smoker population. A total of 300,518 participants (103,288 men and 197,230 women) included in our analysis.
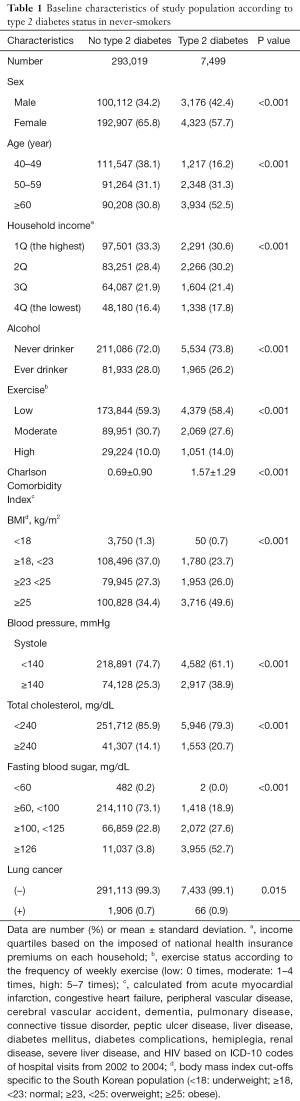
Full table
Unadjusted model shows T2DM associated with incidence of lung cancer based on HRs (Table 2). FBS status at the level of prediabetes and diabetes are associated with lung cancer regardless of diagnosis of T2DM. On the other hands, hypoglycemic levels of FBS are not associated with lung cancer development. Interestingly, FBS levels of prediabetes and diabetes of undiagnosed T2DM group have higher HRs than those of diagnosed T2DM group in the unadjusted model.
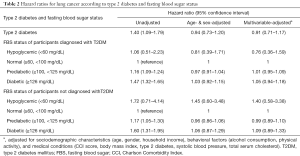
Full table
However, the multivariable model shows that T2DM is not significantly associated with the incident of lung cancer based on HRs (HR =0.91, 95% CI: 0.71 to 1.17; Table 2). Furthermore, abnormal FBS status is also not significantly associated with lung cancer, regardless of participants’ diagnosis of T2DM (Table 2).
Discussion
The participants who were not diagnosed with T2DM between 2003 and 2004, but whose fasting blood glucose had reached diabetic levels at the baseline year estimated that participants might not have kept their fasting time well at the time of the blood test or missed proper diagnosis of diabetes after the test. Therefore, in order to compensate for such ambiguity, we also analyzed the effects of FBS on lung cancer regardless of the diagnosis of T2DM.
Unadjusted analysis of T2DM and FBS level of prediabetes and diabetes on lung cancer development shows significant association. However, all results were statistically insignificant after adjusting for age, gender and other covariables. This suggests that the incidence of lung cancer in nonsmokers can be driven by age regardless of diabetes or blood sugar level.
A never-smoker commonly defined as participants who smoked less than 100 cigarettes over the course of their lifetime by the previous study (5). However, as smoking status data was given by self-reporting questionnaire, we excluded ex-smokers to classify the never-smoker to minimize recall bias in this study.
In this study, data on tumor stage and pathology of tumors could not be obtained, which could not be analyzed. However, since the results of this study included newly diagnosed lung cancer and deaths from lung cancer, the association of T2DM and lung cancer development could be found regardless of tumor stage.
Previous studies have shown the contradictory effects depending on diabetes medication on the incidence of lung cancer (6,7) Although, we did not analysis the effect of each anti-diabetic medication on the incidence of lung cancer, the impact of diabetic FBS levels on lung cancer development was consistently statistically insignificant, regardless of regardless of anti-diabetic medication prescription among never-smokers, based on the multivariable adjusted HR.
A previous review study has identified several factors associated with lung cancer incidence within never-smokers such as: environmental tobacco smoke, occupational exposure to the carcinogen, radon exposure, indoor or outdoor air pollution, as well as genetic factors (5). This study did not take into account the above factors associated with lung cancer in never-smokers, and thus could pose as potential limitations. However, the merits of this study lie in the adjustment of considerable factors such as medical conditions, sociodemographic and behavioral factors within the large-scale longitudinal national cohort data pool. Furthermore, given that the previous study that lung cancer incidence in never-smokers is associated within the Caucasian population (8), this study suggests that lung cancer development in never-smokers in the Korean population is not associated with T2DM or FBS levels.
Acknowledgments
Funding: This study used data from the Korean National Health Insurance Service (NHIS-2017-2-459). The protocol employed in the present study was approved by the Institutional Review Board of Seoul National University Hospital (IRB number: 1703-039-836).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394-424. [Crossref] [PubMed]
- Hall GC, Roberts CM, Boulis M, et al. Diabetes and the risk of lung cancer. Diabetes Care 2005;28:590-4. [Crossref] [PubMed]
- Pallis AG, Syrigos KN. Lung cancer in never smokers: disease characteristics and risk factors. Crit Rev Oncol Hematol 2013;88:494-503. [Crossref] [PubMed]
- Yang WS, Yang Y, Yang G, et al. Pre-existing type 2 diabetes and risk of lung cancer: a report from two prospective cohort studies of 133 024 Chinese adults in urban Shanghai. BMJ Open 2014;4:e004875. [Crossref] [PubMed]
- Subramanian J, Govindan R. Lung cancer in never smokers: a review. J Clin Oncol 2007;25:561-70. [Crossref] [PubMed]
- Tseng C-H. Metformin and lung cancer risk in patients with type 2 diabetes mellitus. Oncotarget 2017;8:41132. [PubMed]
- Ozerlat I. Diabetes therapy and lung cancer. Nature Reviews Endocrinology 2012;8:445. [Crossref] [PubMed]
- Pirie K, Peto R, Green J, et al. Lung cancer in never smokers in the UK Million Women Study. Int J Cancer 2016;139:347-54. [Crossref] [PubMed]


