HER2 driven non-small cell lung cancer (NSCLC): potential therapeutic approaches
Introduction
Lung cancer continues to be the leading cause of cancer-related death, as estimated by the American Cancer Society, responsible for 26% of all female cancer deaths and 29% of all male cancer deaths in the U.S. in 2012 (1). Considering that non-small cell lung cancer (NSCLC) accounts for 80-85% of cases of lung cancer (2) and that significant improvement in survival rates, approximately 17% at 5 years for recently diagnosed NSCLC and less than 4% if presenting with distant metastasis (3), has not been achieved in the last decade with conventional chemotherapy, novel therapeutic approaches are warranted in this field. As a result of these advances, systematic genomic testing for patients with NSCLC is becoming the new standard of care in clinical decision-making, due to the identification of driver mutations that have triggered the development of new molecules targeting these specific alterations in cancer cells. For example, somatic mutations in epidermal growth factor receptor (EGFR) confer greater response rates to tyrosine kinase inhibitors (TKIs) that target the catalytic domain of EGFR, such as erlotinib and gefitinib, compared to standard therapy in advanced NSCLC, 70% vs. 33.2% in first-line trials (4,5). In a similar manner, crizotinib, the anaplastic lymphoma kinase (ALK) tyrosine kinase inhibitor, has demonstrated response rates of approximately 60% with progression-free survival greater than 10 months in those NSCLC characterized by ALK rearrangements (6). These studies have enabled to conclude that both EGFR-mutant and ALK-positive NSCLC constitute two defined subgroups of oncogene-driven tumors with potentially effective targeted therapy. Furthermore, approximately 15-20% of NSCLC diagnosed in Europe and North America bear EGFR mutations or ALK rearrangements (7), enhancing the significance of the development of drugs capable of interfering with their intracellular effects.
Based on these results, the identification of other activating mutations has been pursued in hopes of improving survival in NSCLC by specifically treating these genomic alterations. These potential therapeutic targets include KRAS, BRAF, HER2 and PIK3CA, in addition to ROS1 fusions. KRAS mutations, in codons 12, 13 and 61, reported in approximately 20% of cases of lung adenocarcinomas, predict negative outcome in terms of response to EGFR TKIs. No targeted therapies have demonstrated an increase in overall survival in KRAS-mutant NSCLC, although selumetinib, an inhibitor of MAPK extracellular signal-regulated kinase (MEK) 1/2 (downstream of KRAS), in combination with docetaxel in previously treated advanced NSCLC has shown promising results in a recent phase 2 trial (8).
Regarding activating mutations in BRAF, HER2 and PIK3CA, incidence reported for each group ranges from 1-4%, a lower although significant frequency that is encouraging further investigation of these genetic alterations and consequent therapeutic implications. HER2 mutations in NSCLC constitute a clear molecular target, particularly in a subset of patients with distinct clinical features, including female non-smokers with adenocarcinomas, similar to those patients with EGFR-mutant lung cancer. Here, we seek to review the characteristics of HER2 mutations that enable interaction with molecules that specifically target these receptors in lung adenocarcinomas, as well as the results of preliminary studies that assess the efficacy of anti-HER2 therapy applied to NSCLC.
Tumorigenesis induced by HER2 mutations
HER2 [also known as epidermal growth factor receptor-2 (EGFR2), ERBB2 or NEU] is a member of the ERBB receptor tyrosine kinase family, which includes 3 additional members; EGFR (HER1/ERBB1), HER3 (ERBB3) and HER4 (ERBB4). The binding of ligands to the extracellular domain of EGFR, HER3 and HER4 induces homo- and heterodimerization of these receptors, catalytically activating a cascade of intracellular pathways involved in cellular proliferation, differentiation and migration. These reactions are induced by cytoplasmic signal transducers such as PLC-γ1, Ras-Raf-MEK-MAPKs, phosphatidylinositol-3 kinase (PI3K), Src or the signal transducers and activators of transcription (STATs). However, no ligand has been described for HER2, regardless of structural resemblance between ERBB receptors. In fact, HER2 has been identified as the preferred binding partner of the other ERBB receptors, in particular, of EGFR with formation of HER2/EGFR heterodimers with increased potential for signaling than EGFR homodimers (9). This unique characteristic of HER2 has been partially attributed to its increased flexibility due to a glycine-rich region following the alpha-helix C of HER2, which explains its low intrinsic catalytic activity and less stable conformation when activated (10). Consequently, HER2 overexpression potentiates EGFR signaling which relates to the increased response in EGFR-positive NSCLC with HER2 overexpression to erlotinib or gefitinib (11), specific inhibitors of active EGFR, but not of HER2 or inactive EGFR.
HER2 gene, regulated by overexpression and/or gene amplification, has been proven important in many cancers, including breast and gastric cancer, in which overexpression of HER2 confers poor prognosis although it relates to possible benefit from specific anti-HER2 therapy. With the arrival of trastuzumab, a humanized monoclonal IgG1 that targets the extracellular domain of HER2, and its effect in combination with cytotoxic chemotherapy on survival rates of breast and gastric cancer with overexpression of HER2, a new door in molecular-targeted therapy was opened. However, although HER2 overexpression and amplification has been described in 6-35% and in 10-20%, respectively, of NSCLC patients, the first clinical trials including patients treated with trastuzumab in addition to gemcitabine-cisplatin or to docetaxel, failed to demonstrate benefit in survival in HER2 IHC-positive patients (12,13).
These findings triggered investigation of activating mutations in the tyrosine kinase domain of HER2 gene, first described in 2004. HER2 mutations have been reported to exist in up to 4% of NSCLC and are more common in Asians, never smokers, women and adenocarcinomas (14), characteristically similar to patients with EGFR mutations. These mutations occur in the first four exons of the tyrosine kinase domain (exons 18-21), including the most frequently observed alteration, a 12-bp duplication/insertion of the amino acid sequence YVMA in exon 20 at codon 776 (HERYVMA). The mutated region of exon 20 in the HER2 gene corresponds to the nine codon region in exon 20 of the EGFR gene, where duplications and insertions have also been described, resulting in conformational changes of the tyrosine kinase domain that lead to narrowing of the ATP binding cleft and, consequently, increased kinase activity compared to wild-type receptors (HERWT). In vitro studies have demonstrated that HERYVMA induces ligand-independent transphosphorylation and stronger association with signal transducers that mediate cell proliferation, motility and survival processes than HERWT (15). In fact, HERYVMA activates EGFR in absence of ERBB ligands and EGFR kinase activity, which explains that EGFR TKIs erlotinib and gefitinib have no effect on EGFR and HER2 phosphorylation in HERYVMA cells. However, when the effect of trastuzumab in cell proliferation was tested in these in vitro studies, inhibition was achieved in presence of HERYVMA but not cells overexpressing HERWT, findings consistent with the reported inability of the IgG1 to bind with EGF and or EGFR/HER2 heterodimers (16). Therefore, authors concluded that tumor cells harboring HER2 mutations are resistant to EGFR inhibitors although remain sensitive to HER2 inhibitors and dual EGFR/HER2 inhibitors.
Epidemiology of HER2 mutations in lung cancer
Up to date, few studies regarding HER2 mutations in NSCLC have been published, primarily in Asian patient populations in which never smokers constitute a greater percentage of lung cancer patients (approximately 30%) compared to North American and European populations (10%). Incidence of HER2 mutations has been reported in 2-5% of NSCLC adenocarcinomas (Table 1). In a retrospective study of pulmonary resection samples obtained at the Fudan University Shanghai Cancer Centre (17), a total of 202 patients, never smokers, with lung adenocarcinoma that had not received neoadjuvant chemotherapy, were included. The median age at diagnosis was 57.3 years and no significant differences were observed in age, stage or degree of tumor differentiation between males and females. Of these samples, 89.1% harbored known oncogenic driver mutations in EGFR (75.25%), HER2 (5.94%), ALK fusion (4.95%), KRAS (1.98%), ROS1 fusion (0.99%). Patients with no identified driver mutation were diagnosed at a younger age. 12 samples with HER2 kinase domain mutations were detected, including 11 exon 20 insertions and 1 L775P point mutation.
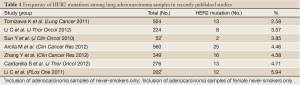
Full Table
Recently, the Memorial Sloan Kettering Cancer Centre (MSKCC) group published the largest assessment to date of HER2 mutations in predominantly Caucasian population (18). Of 560 lung adenocarcinoma samples that resulted negative for EGFR and KRAS major mutations tested previously, 26 HER2 mutations in 25 cases were identified (5%), all mutually exclusive with point mutations in EGFR, KRAS, BRAF, NRAS, PI3KCA, MEK1 and AKT mutations as well as ALK rearrangements. No HER2 mutations were detected among 104 squamous cell carcinomas and 6 small-cell carcinomas tested. 92% (24/26) of these HER2 mutations were in-frame insertions in exon 20 (from 3 to 12 bp) between codons 775 and 881, of which the most common (83%) was the 12-bp duplication/insertion of YVMA at codon 775. The other two cases were point mutations, L775S and G776C. Median follow-up after diagnosis of advanced disease was 19 months for all patients. No significant differences in overall survival were described between HER2 and other molecular subsets. Morphologically, 92% were moderately or poorly differentiated adenocarcinomas. An additional analysis was performed to assess for HER2 gene copy number alterations by FISH in 11 HER2 mutated and 39 WT cases. None of HER2-mutant specimens were positive for HER2 amplification; 18% presented high polysomy (>4 copies of HER2 in >40% of cells) and 73% low polysomy. Amplification of HER2 was detected in one case, in the WT group, and interestingly this case was also found to harbor an EGFR exon 19 deletion. Therefore, HER2 mutation was not associated with concurrent HER2 amplification.
In this study, the overall prevalence of HER2 mutations was estimated to be approximately 2%, similar to statistics obtained in smaller European studies (19). In addition, HER2 mutations were most frequent among never-smokers (P<0.0001) although there were no associations with gender, race or stage of disease.
Therapeutic implications: HER2-targeted therapy in NSCLC
HER2 overexpression and gene amplification has been observed in breast, gastric and ovarian malignancies, inducing sensitivity to HER2-targeted drugs including trastuzumab, pertuzumab, lapatinib and T-DM1. Both amplification and high copy number gains have also been identified in NSCLC, although first clinical trials with anti-HER2 therapies in unselected patients failed to demonstrate survival benefit in HER2 positive NSCLC (defined by immunohistochemistry) (12,20). However, there is new hope that HER2 mutations may be more relevant in lung carcinogenesis than HER2 amplification or overexpression. Based on previous in vitro and in vivo studies, Cappuzzo et al. showed that lung cancer harboring the HER2 Gly776Leu mutation responded to treatment with trastuzumab and paclitaxel in a patient with chemotherapy-refractory lung adenocarcinoma (21).
Considering that HER2-mutant NSCLC may benefit from HER2 inhibition or dual EGFR/HER2 inhibition, but not single blockage of EGFR, novel TKIs simultaneously targeting EGFR/HER2 have been investigated. Transgenic mice models with induced expression in lung epithelium of the most common HER2 mutant, HER2YVMA, developed lung adenosquamous carcinomas in distal and proximal bronchioles (22). In these models, treatment with erlotinib, trastuzumab, BIBW2992 and/or rapamycin revealed that the combination of BIBW2992 (afatinib), an irreversible dual TKI targeting both EGFR and HER2, and rapamycin, an inhibitor of the downstream effector protein mTOR, produced the most significant shrinkage (50.1±27.4% tumor regression measured by MRI) of tumor specimens. In addition, immunohistochemical analysis of these tumors treated with BIBW2992 and rapamycin proved this combination to be the most effective regimen for inhibition of upstream and downstream signaling of both the ERBB/PI3K/mTOR and the MAPK signaling pathways. Surprisingly, a relatively low effect was observed in HER2YVMA models treated with trastuzumab, with an average tumor regression of 13.59% (±10.89%), which was theoretically explained by postulating that trastuzumab is capable of inhibiting phosphorylation of membranous HER2 but unable to inhibit intracellular HER2 signaling associated with Golgi, endoplasmic reticulum, and other transport vesicles. Interestingly, continuous expression of HER2YVMA was proven necessary for tumor maintenance, indicating that HER2 is of great importance in lung adenosquamous tumorigenesis.
Case reports of afatinib in patients with HER2 mutant NSCLC have revealed promising results (23). Of patients who were included in an exploratory Phase II study of afatinib, five patients with non-smoking history and metastatic lung adenocarcinomas were identified to harbor HER2 mutations in cancer specimens. Three of these were evaluated, observing objective response to afatinib in all cases.
Neratinib, an irreversible pan ERBB-receptor family inhibitor, has been studied in a phase II trial in patients with advanced NSCLC who progressed following erlotinib or gefitinib (24). Three subgroups, EGFR mutant, wild-type EGFR and EGFR TKI naive- adenocarcinoma with light smoking history, were compared obtaining objective response rates of 3.4%, 0% and 0%, respectively. Only a small subgroup of patients with G719X mutation at exon 18 of EGFR-positive tumors, refractory to reversible TKIs, benefited from neratinib. Based on these results, neratinib is no longer in development for NSCLC although investigation in HER2-positive breast cancer continues.
PF00299804 (dacomitinib), another irreversible TKI targeting ERBB family members EGFR, HER2 and HER4, is being evaluated in patients with NSCLC. Preliminary data of dacomitinib in the HER2-mutant cohort reveal a 14% (3 of 22) partial response rate and 27% of these patients (6 of 22) have maintained stable disease to date (25).
In addition to TKIs, other molecules targeting EGFR and HER2 receptors have been developed. Considering that the heat shock protein 90 (Hsp90) chaperone stabilizes various oncogenic kinases necessarily involved in signal transduction and proliferation of lung carcinoma cells, when Hsp90 was demonstrated to interact with mutant EGFR, inhibition of these chaperones became a new potential therapeutic approach (26). NSCLC with activating EGFR mutations that develop acquired resistance to EGFR TKI after treatment with erlotinib or gefitinib, have been proven sensitive to Hsp90 inhibitors both in NSCLC cell lines in vitro and in vivo (27). Other targets of Hsp90 include mutant HER2, mutant BRAF or mutant or overexpressed MET; therefore, adenocarcinomas harboring HER2 mutations may benefit from disruption of chaperone function. In fact, ganetespib, a novel non-geldanamycin potent Hsp90 inhibitor that impedes binding of Hsp90 to its co-chaperone, p23, has been proven effective in NSCLC cell lines in mice models driven by mutations in both EGFR and HER2YVMA (28). These promising data support further investigation in clinical trials.
Conclusions
The discovery of oncogenic driver mutations in NSCLC is leading to the development of new therapies targeting specific molecular alterations. Detection of EGFR mutations and ALK rearrangements in tumor specimens of recently diagnosed NSCLC is currently standard of care, in order to identify subsets of patients that may respond to TKIs, such as erlotinib or gefitinib and crizotinib, respectively. Considering the prevalence of lung adenocarcinoma and clinical relevance of other mutations in NSCLC, including HER2, at diagnosis of this subgroup of lung cancer patients, we suggest expanding systematic genotype testing to include detection of these molecular alterations. In comparison with other types of cancer (i.e. breast, gastric) in which HER2 overexpression and gene amplification is associated to greater response to anti-HER2 drugs such as trastuzumab, first clinical trials in HER2 IHC-positive NSCLC failed to demonstrate benefit in the addition of trastuzumab to chemotherapy. However, HER2 mutations are thought to play a more significant role in lung cancerogenesis than overexpression or gene amplification, achieving promising results with trastuzumab in advanced HER2-mutant NSCLC. Therefore, identification of HER2 mutations, rather than HER2 IHQ-positive cancer specimens, should be studied in recently diagnosed stage IV NSCLC patients.
In addition, considering that cancer cells harboring HER2 mutations may respond to both HER2 inhibitors and dual EGFR/HER2 inhibitors, newer agents, including dacomitinib and afatinib, are currently under investigation in clinical trials specifically for this indication. Phase II studies have demonstrated promising initial results, although further investigation is necessary. Inhibition of chaperones to oncogenic kinases has revealed favorable results in preclinical models, constituting a new therapeutic strategy to be explored in both EGFR- and HER2-mutant NSCLC.
In summary, mutations in the tyrosine kinase domain of HER2 identify a subset of NSCLC adenocarcinomas, with a greater prevalence among never-smokers, which may respond to novel agents that specifically target this alteration. HER2 mutations are mutually exclusive with other driver mutations and are independent of HER2 gene amplification. Considering the prevalence of lung adenocarcinomas and given the availability of standard and investigational therapies targeting HER2, clinical genotyping of these tumors should include HER2.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin 2012;62:10-29.
- Peters S, Adjei AA, Gridelli C, et al. Metastatic non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2012;23:vii56-64.
- Cetin K, Ettinger DS, Hei YJ, et al. Survival by histologic subtype in stage IV nonsmall cell lung cancer based on data from the Surveillance, Epidemiology and End Results Program. Clin Epidemiol 2011;3:139-48.
- Petrelli F, Borgonovo K, Cabiddu M, et al. Efficacy of EGFR tyrosine kinase inhibitors in patients with EGFR-mutated non-small-cell lung cancer: a meta-analysis of 13 randomized trials. Clin Lung Cancer 2012;13:107-14.
- Rosell R, Carcereny E, Gervais R, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol 2012;13:239-46.
- Kwak EL, Bang YJ, Camidge DR, et al. Anaplastic lymphoma kinase inhibition in non-small-cell lung cancer. N Engl J Med 2010;363:1693-703.
- Cardarella S, Ortiz TM, Joshi VA, et al. The introduction of systematic genomic testing for patients with non-small-cell lung cancer. J Thorac Oncol 2012;7:1767-74.
- Jänne PA, Shaw AT, Pereira JR, et al. Selumetinib plus docetaxel for KRAS-mutant advanced non-small-cell lung cancer: a randomised, multicentre, placebo-controlled, phase 2 study. Lancet Oncol 2013;14:38-47.
- Lenferink AE, Pinkas-Kramarski R, van de Poll ML, et al. Differential endocytic routing of homo- and hetero-dimeric ErbB tyrosine kinases confers signaling superiority to receptor heterodimers. EMBO J 1998;17:3385-97.
- Aertgeerts K, Skene R, Yano J, et al. Structural analysis of the mechanism of inhibition and allosteric activation of the kinase domain of HER2 protein. J Biol Chem 2011;286:18756-65.
- Cappuzzo F, Varella-Garcia M, Shigematsu H, et al. Increased HER2 gene copy number is associated with response to gefitinib therapy in epidermal growth factor receptor-positive non-small-cell lung cancer patients. J Clin Oncol 2005;23:5007-18.
- Gatzemeier U, Groth G, Butts C, et al. Randomized phase II trial of gemcitabine-cisplatin with or without trastuzumab in HER2-positive non-small-cell lung cancer. Ann Oncol 2004;15:19-27.
- Krug LM, Miller VA, Patel J, et al. Randomized phase II study of weekly docetaxel plus trastuzumab versus weekly paclitaxel plus trastuzumab in patients with previously untreated advanced nonsmall cell lung carcinoma. Cancer 2005;104:2149-55.
- Li C, Sun Y, Fang R, et al. Lung adenocarcinomas with HER2-activating mutations are associated with distinct clinical features and HER2/EGFR copy number gains. J Thorac Oncol 2012;7:85-9.
- Wang SE, Narasanna A, Perez-Torres M, et al. HER2 kinase domain mutation results in constitutive phosphorylation and activation of HER2 and EGFR and resistance to EGFR tyrosine kinase inhibitors. Cancer Cell 2006;10:25-38.
- Agus DB, Akita RW, Fox WD, et al. Targeting ligand-activated ErbB2 signaling inhibits breast and prostate tumor growth. Cancer Cell 2002;2:127-37.
- Li C, Fang R, Sun Y, et al. Spectrum of oncogenic driver mutations in lung adenocarcinomas from East Asian never smokers. PLoS One 2011;6:e28204.
- Arcila ME, Chaft JE, Nafa K, et al. Prevalence, clinicopathologic associations, and molecular spectrum of ERBB2 (HER2) tyrosine kinase mutations in lung adenocarcinomas. Clin Cancer Res 2012;18:4910-8.
- Buttitta F, Barassi F, Fresu G, et al. Mutational analysis of the HER2 gene in lung tumors from Caucasian patients: mutations are mainly present in adenocarcinomas with bronchioloalveolar features. Int J Cancer 2006;119:2586-91.
- Langer CJ, Stephenson P, Thor A, et al. Trastuzumab in the treatment of advanced non-small-cell lung cancer: is there a role? Focus on Eastern Cooperative Oncology Group study 2598. J Clin Oncol 2004;22:1180-7.
- Cappuzzo F, Bemis L, Varella-Garcia M. HER2 mutation and response to trastuzumab therapy in non-small-cell lung cancer. N Engl J Med 2006;354:2619-21.
- Perera SA, Li D, Shimamura T, et al. HER2YVMA drives rapid development of adenosquamous lung tumors in mice that are sensitive to BIBW2992 and rapamycin combination therapy. Proc Natl Acad Sci U S A 2009;106:474-9.
- De Grève J, Teugels E, Geers C, et al. Clinical activity of afatinib (BIBW 2992) in patients with lung adenocarcinoma with mutations in the kinase domain of HER2/neu. Lung Cancer 2012;76:123-7.
- Sequist LV, Besse B, Lynch TJ, et al. Neratinib, an irreversible pan-ErbB receptor tyrosine kinase inhibitor: results of a phase II trial in patients with advanced non-small-cell lung cancer. J Clin Oncol 2010;28:3076-83.
- Kris M, Goldberg Z, Jänne P, et al. Dacomitinib (Pf-00299804), an Irreversible Pan-HER Tyrosine Kinase Inhibitor, for First-Line Treatment of EGFR-Mutant or HER2-Mutant or -Amplified Lung Cancers. Ann Oncol 2012;23:ix401-ix402.
- Shimamura T, Shapiro GI. Heat shock protein 90 inhibition in lung cancer. J Thorac Oncol 2008;3:S152-9.
- Kobayashi N, Toyooka S, Soh J, et al. The anti-proliferative effect of heat shock protein 90 inhibitor, 17-DMAG, on non-small-cell lung cancers being resistant to EGFR tyrosine kinase inhibitor. Lung Cancer 2012;75:161-6.
- Shimamura T, Perera SA, Foley KP, et al. Ganetespib (STA-9090), a nongeldanamycin HSP90 inhibitor, has potent antitumor activity in in vitro and in vivo models of non-small cell lung cancer. Clin Cancer Res 2012;18:4973-85.


