Tumor heterogeneity: evolution through space and time in EGFR mutant non small cell lung cancer patients
Introduction
Non-small cell lung cancer (NSCLC) is the leading cause of cancer mortality worldwide, and traditional chemotherapeutic drugs are only modestly effective. Most lung cancer patients usually present with advanced stage disease, where the efficacy of chemotherapy is low, with a 5-year survival rate lower than 15% (1).
The discovery of mutated oncogenes encoding activated signaling molecules that drive cellular proliferation and promote tumor growth has led to the development of more effective and less toxic targeted therapies for NSCLC patients. Particularly, NSCLC patients with mutations in epidermal growth factor receptor (EGFR) gene have dramatic responses and better outcome with the EGFR tyrosine kinase inhibitors (TKI) gefitinib and erlotinib (1-9).
The EGFR is a well characterized mutated oncogene in NSCLC that is associated predominantly with adenocarcinoma histology. EGFR-mutated tumors depend to EGFR signaling for their proliferation and survival. Nearly 90% of lung-cancer-specific EGFR mutations comprise a leucine-to-arginine substitution at position 858 (L858R) and deletion in exon 19 that affect the conserved sequence LREA (delE746-A750) (3,8,10,11).
Unfortunately, despite the dramatic efficacy of EGFR TKI in NSCLC patients with EGFR activating mutations, all patients eventually acquire resistance, with progression of disease occurring in patients around 10-13 months after starting treatment (2,7,12). There are two main mechanisms of resistance to EGFR TKI: the lack of an initial response to therapy, also called de novo or primary resistance to EGFR TKI, and resistance that develops following an initial response to EGFR TKI, also called acquired resistance to EGFR TKI.
To discover those mechanisms involved in EGFR TKI resistance is a significant challenge in order to develop more effective targeted therapies alone or in combination with EGFR TKI for patients with NSCLC and EGFR mutations. In this article we review the molecular basis of resistance of EGFR mutant NSCLC patients to EGFR TKI and rebiopsy strategies to better understand the underlying molecular basis of resistance.
Primary resistance to EGFR TKIs
Patients with NSCLC and EGFR activating mutation will experience significant tumor regression with EGFR TKI in approximately 70% of cases (5), which means a lack of an initial response in about 30% of patients. Those patients will present primary or de novo resistance to EGFR TKI.
To date, two main mechanisms of primary resistance to EGFR TKI in EGFR mutant NSCLC patients have been described: first, the presence of secondary alterations in EGFR that prevent inhibition of EGFR by an EGFR TKI (also known drug resistant EGFR mutation), and second, the presence of additional genetic alternations that occur together with EGFR mutation.
Secondary alterations in EGFR
EGFR exon 20 insertions
EGFR Exon 20 insertions comprise approximately 4% of all EGFR mutant NSCLC (13) and are associated with lower sensitivity to the reversible EGFR TKIs both in preclinical models and in patients that have experienced a lack of response when treated with gefitinib or erlotinib (14-16). The irreversible EGFR TKIs could be more effective in these mutations (15,17-19).
EGFR T790M (c.2369C>T) mutation in non-small cell lung cancer
The T790M mutation results in an amino acid substitution at position 790 in EGFR, from a threonine (T) to a methionine (M). This gatekeeper mutation also occurs within exon 20, which encodes part of the kinase domain EGFR and alters the binding of EGFR TKI to the ATP-binding pocket, and therefore EGFR TKI are unable to block EGFR signalling (20-22). These pretreatment T790M mutations generally occur together with another EGFR sensitizing mutation and have been found to be associated with decreased sensitivity to EGFR TKIs (16). Additionally, the baseline T790M mutations may be present as an underlying germline mutation at a low frequency (0.5% of never smokers with lung cancer) (23) and may be associated with familial cancer syndromes (24).
Rosell et al. assessed the T790M mutation in pretreatment diagnostic specimens from 129 EGFR TKI treated advanced NSCLC patients with EGFR mutations, and found that EGFR T790M mutation was present in 45 of 129 patients (35%). Progression-free survival was 12 months in patients with and 18 months in patients without the T790M mutation (P=0.05). Additionally, it was found that low BRCA-1 levels neutralized the negative effect of the T790M mutation and were associated with longer progression-free survival to erlotinib, whereas high levels of BRCA-1 may lead to de novo resistance through increased DNA damage repair capacity, suggesting that pretreatment assessment of both T790M mutation and BRCA1 expression could be useful to predict outcome (25). Additionally, in the EURTAC trial the T790M mutation was detected in 38% of the pre-treatment specimens analysed (26).
Fujita et al. evaluated the incidence of T790M in pretreatment tumor specimens using highly sensitive colony hybridization technique and was detected in 30/38 resected tumor tissues of patients with the EGFR mutation (79%). The median time to treatment failure was 9 months for the patients with pretreatment T790M and 7 months for the patients without the T790M mutation (P=0.44), and suggested that patients with high proportion of T790M allele may have a relatively favorable prognosis (27).
In addition to EGFR T790M, primary EGFR TKI resistance may also be due to other secondary mutations in EGFR (e.g., D761Y) that can occur concurrent with an activating EGFR kinase domain mutation (e.g., L858R) (28).
Genetic alternations with EGFR mutations
Other genetic alterations may occur together with EGFR mutation causing EGFR TKI resistance by preserving cell survival even with EGFR inhibition. These additional genetic alterations that promote EGFR pathway include:
Activation of phosphoinositide-3-kinase (PI3K)/AKT signaling
Phosphatase and tensine homolog (PTEN) acts as a tumor suppressor by negatively regulating the PI3K/AKT signaling pathway. In preclinical studies, loss of PTEN was associated with decreased sensitivity of EGFR mutant lung tumors to EGFR TKI by increased activity of the PI3K-AKT pathway, and degradation of activated EGFR (29,30).
Somatic mutations in PIK3CA have been found in 1-3% of all NSCLC (31,32). These mutations usually occur within two “hotspot” areas within exon 9 (the helical domain) and exon 20 (the kinase domain). Preclinical data has shown that introduction of activating PIK3CA mutants into EGFR mutant lung cancer cell lines confers resistance to EGFR TKI (33).
Crosstalk with the IGF1R pathway
Resistance to EGFR TKI in cell lines with EGFR activating mutations through crosstalk with the IGF1R pathway has been observed through in preclinical models. For example, some EGFR-mutant cells undergo only G1 cell cycle phase arrest in the presence of erlotinib, but undergo apoptosis when co-treated with an IGF1R-specific antibody (34). In another study, EGFR mutant NSCLC cell lines persisting after EGFR TKI treatment were enriched for a drug-tolerant subpopulation that may have existed prior to treatment that showed a distinct chromatin state that is regulated by IGF1R signalling (35).
Activation of NFκB signaling
NFκB is a protein complex that controls the transcription of DNA. NFκB signaling has been associated with cancer and inflammation (36), and it has also been suggested that activation of NFκB signaling may cause primary resistance to EGFR TKI treatment in EGFR mutant lung cancer patients.
Bivona et al. used a cell line (H1650) with EGFR mutation but resistant to EGFR TKI and showed that inhibition of the NFκB pathway enhanced cell death by EGFR TKI whereas activation of NFκB rescued EGFR-mutant lung cancer cells from EGFR TKI treatment. Additionally, genetic or pharmacologic inhibition of NFκB enhanced erlotinib-induced apoptosis in erlotinib-sensitive and erlotinib-resistant EGFR-mutant lung cancer models, and increased expression of the NFκB inhibitor IκB, predicted for improved response and survival in EGFR-mutant lung cancer patients treated with EGFR TKI. Importantly, IκB status was not predictive of outcomes in EGFR mutant lung cancer patients treated with surgery or chemotherapy, indicating NFκB signaling is specific biomarker of EGFR TKI response in this patient population (37). These data identify NFκB as a potential drug target, together with EGFR, in EGFR-mutant lung cancers.
High BIM expression levels
BIM, also known as BCL2-like 11, is a proapoptotic protein that is overexpressed in different malignancies (38,39). Various chemotherapeutic agents use BIM as a mediating executioner of cell death. Hence, BIM suppression supports metastasis and chemoresistance. BIM upregulation is required for apoptosis induction by EGFR-TKIs in EGFR-mutant NSCLC. Low BIM mRNA levels could lead to gefitinib resistance in NSCLC with EGFR mutations and could be a marker of primary resistance. The extracellular regulated kinase (ERK) pathway also negatively regulates BIM expression in NSCLC with EGFR mutations (40-42). Components that cause induction of BIM may have a role to overcome resistance to EGFR TKI in NSCLC with EGFR mutations. Recent studies have showed that HDAC inhibition can epigenetically restore BIM function in vitro and death sensitivity of EGFR-TKI, in cases of EGFR mutant NSCLC where resistance to EGFR-TKI is associated with a common BIM polymorphism (43).
Treatment approaches to overcome primary resistance
For lung cancer patients harboring secondary alterations in EGFR, more effectively EGFR TKI is needed. Second-generation irreversible EGFR TKI have shown to be more active targeting T790M or EGFR exon 20 insertion mutation than gefitinib or erlotinib (44-46). Additionally, the Spanish Lung Cancer Group is conducting a phase Ib/IIb Study to evaluate the role of gefitinib in combination with olaparib in NSCLC patients with EGFR mutation to overcome primary resistance in those patients with high BRCA1 levels (NCT01513174). For lung cancer patients harboring other genetic alterations with EGFR mutation the use of polytherapy could overcome primary resistance. For example, a phase II trial of erlotinib and AT-101 (BCL-2 pan inhibitor) in NSCLC patients with EGFR mutations has been performed, although no results have been presented, yet (NCT00988169).
Additionally, a combination of an EGFR TKI with PI3K-AKT, IGFR, NFκB or BIM inhibitors could also play a role in those alterations co-occur causing EGFR TKI resistance.
Acquired resistance to EGFR TKI
Several mechanisms of acquired resistance to EGFR TKI in EGFR mutant NSCLC patients have been reported, which could be grouped in four main categories: first, the presence of secondary mutations in EGFR; second, the presence by-pass tracks activation; third a phenotypic transformation; and fourth, additional genetic alternations that occur together with EGFR mutation. Up to 30% of cases are still unexplained.
Second-site mutations in EGFR
Approximately 50-60% of cases with acquired resistance to EGFR TKI therapy have a second-site mutation T790M (“gatekeeper mutation”) in the kinase domain of EGFR that coexists with the EGFR activating mutation (21,47). Conversely to primary T790M mutation, acquired resistance by T790M mutation identifies a subset of EGFR-mutant lung cancers with indolent growth in preclinical (48) and clinical set (49).
The subclonal populations of EGFR mutant tumor cells with and without the EGFR T790M can coexist in an EGFR mutant NSCLC with acquired resistance to EGFR TKI. This heterogeneity would explain both the “flare” phenomenon (rapid tumor regrowth upon withdrawal of an EGFR TKI) observed upon discontinuation of an EGFR TKI and also the finding that EGFR mutant NSCLC patients may respond to subsequent EGFR TKI treatment after initial discontinuation of therapy (50-53).
In addition to EGFR T790M mutation, there are other mutations that have been associated with acquired EGFR TKI resistance: T854A in exon 21 (54), L747S (55), and D761Y (28), both in exon 19. However, the frequency of all such mutation appears to be very low in comparison with the T790M mutation.
By-pass tracks activation
Other mechanism of acquired resistance to EGFR TKI is the activation of parallel pathways in which the key downstream targets of EGFR are activated independently of EGFR. These mechanisms include MET amplification and HGF overexpression. Amplification of the receptor tyrosine kinase MET leads EGFR inhibitor resistance by causing phosphorylation of ERBB3, which in turn sustains the activation of the PI3K/Akt signal downstream, providing a bypass signalling even in the presence of EGFR inhibitor. MET amplification was detected in 22% of lung cancer specimens that developed acquired resistance to EGFR TKI and inhibition of both EGFR and MET was required to kill the resistant cells, suggesting a persistent oncogenic addiction to EGFR pathway beyond to acquired resistance to EGFR TKI (56-58). In the clinic, MET amplification was reported in 4% of patients. The prevalence of MET-dependent resistance may depend upon the assay used (59).
Although MET amplification can occur with the EGFR T790M mutation, about 60% of MET amplification is independent of T790M mutation. There is an inverse relationship between the presence of T790M and MET gene copy number, suggesting a complementary role of the two mechanisms in the acquisition of resistance. In preclinical models, MET inhibitors may be able to overcome MET-mediated resistance, even in cells that harbour the T790M mutation (60). Concurrent inhibition therapy might be essential for outcome improvement (61). MET activation by overexpression of its ligand, HGF, also induced drug resistance in vitro and in vivo through GAB1 signalling, which directly activates PI3K/Akt pathway (62). In patients with paired tumor specimens, HGF expression was higher in drug-resistant specimens than in the pretreatment specimens (P=0.025) (63) and in other study with 23 acquired resistance tumors, high-level HGF expression was detected in higher proportion than T790M mutation (62). Japanese patients with weak HGF expression by immunohistochemistry tend to have lower 5-year OS than those with overexpression (22.2% vs. 75%, P=0.259) (64). Of note, MET amplification has also been observed in EGFR mutant NSCLC patients prior to EGFR TKI and was associated with the development of acquired resistance to EGFR TKIs (60), suggesting that EGFR TKI may select for preexisting cells with MET amplification during the acquisition of EGFR TKI resistance.
Phenotypic transformation
This acquired resistance mechanism includes the histological transformation to small cell lung cancer (SCLC) and the epithelial to mesenchymal transition (EMT), with an incidence of 14% and 5%, respectively (58). These new SCLC retain the original EGFR-sensitizing mutation and respond to standard small cell carcinoma chemotherapy, but the exact mechanism for this histological transformation is unknown.
EMT is a phenomenon characterized in which the cancer cell looses its epithelial morphology and develops a more spindle-like mesenchymal morphology with often associated with a shift in expression of specific proteins (for example, loss of E-cadherin and gain of vimentin) resulting in a more invasiveness phenotype (65). The exact mechanism for the acquisition of the EMT phenotype remains unclear; some studies have found an upregulation of NOTCH-1 expression (66), the aberrant expression of transforming growth factor (TGF)-β (67,68), and phosphorylation of MEK (69). Increased expression of E-cadherin, has been associated with clinical activity of EGFR TKI in NSCLC patients (70,71). EMT has been also associated with acquired resistance to EGFR TKI in preclinical models (65,71) as well as in several studies (58). It is unknown if mesenchymal-like cells in the acquired resistant tumors are exist prior to therapy or are induced upon drug treatment. It has been recently described that activation of the AXL receptor tyrosine kinase by overexpression or upregulation of its ligand GAS6 confers acquired resistance to EGFR TKI in preclinical models, and the inhibition of AXL restored erlotinib sensitivity. Upregulation of AXL was associated with the development of an EMT in EGFR mutant NSCLC with acquired resistance. Approximately 20% of the EGFR TKI resistant tumors showed increased AXL expression (72).
Additional genetic alternations
PIK3CA mutation
Mutation in PIK3CA was identified in 5% of EGFR mutant lung cancers that developed acquired EGFR TKI resistance as well as in preclinical models (58).
PTEN mutation
In preclinical models, loss of PTEN expression contributes to TKI resistance in NSCLC (73). Cells with knockdown of PTEN, with constitutive PI3KCA activation, have a deficient homologous recombinant DNA repair and increased sensitivity to cisplatin and PARP inhibitors (74).
HER2 amplification
HER2 amplification has been recently detected in 12% of tumors with acquired resistance to EGFR TKI, and only in 1% of untreated EGFR mutant NSCLC cells. This new mechanism of acquired resistance was exclusive with T790M mutation (75). Interestingly, in preclinical models the combination of afatinib plus cetuximab significantly inhibited HER2 phosphorylation. These results implicate HER2 as a novel protein involved in the sensitivity or resistance of EGFR mutant NSCLC providing a rationale to assess its status and target HER2 in such tumors.
MAPK1 amplification
MAPK1 amplification was described in approximately 5% of clinical specimens from patients with acquired resistance to EGFR TKI treatment and was mutually exclusive with the T90M mutation or MET amplification (76).
BRAF mutation
RAS pathway mutations are rare, but BRAF mutations (V600E, G469A) can occur in 1% of tumors with acquired resistance to EGFR TKI (77).
JAK2
In a preclinical cell line model, the activation of JAK2 (an upstream STAT signal pathway) caused acquired EGFR TKI resistance. Combined treatments of erlotinib plus a JAK2 inhibitor (JSI-124) restored sensitivity to erlotinib in PC-9/ERB3 cells and reduced tumors in a murine xenograft model (78).
IGFR
In vitro data showed that the increased IGF-1R signalling through the loss of IGF inhibitory proteins may also mediate resistance to EGFR TKI by activating downstream targets that bypass dependency in EGFR (79).
Loss of activating EGFR mutant gene
Loss of activating EGFR mutant gene contributes to acquire resistance to EGFR TKI in lung cancer cells. This loss of addiction to mutant EGFR resulted in gain of addiction to both HER2/HER3 and PI3K/AKT signalling to acquire EGFR TKI resistance (80).
Treatment approaches to overcome acquired resistance
Given this role of persistent EGFR signalling in causing resistance to TKI, a second generation irreversible EGFR TKI bind to a different EGFR tyrosine kinase domain have shown activity against lung cancer cells harboring both EGFR activation mutations and the T790M resistance-mutation (17,45,81,82). A phase III trial of afatinib versus placebo in patients with acquired resistance to EGFR TKI demonstrated a 2-month improvement in progression free survival; although no significant benefit in overall survival was observed (83).
A more recent strategy for intensification of EGFR inhibition has been the addition of monoclonal antibodies targeting EGFR, such as cetuximab. Combined treatment with afatinib and cetuximab induced regression in T790M transgenic murine and mice models with erlotinib resistant lung tumors (84). This synergistic activity has been confirmed in phase I/II clinical trial, with a response rate of 32% in heavily pre-treated population with T790M-positive and T790M-negative tumors and a median Progression free survival of 4.67 months (85). Erlotinib plus cetuximab has showed to overcome T790M-mediated drug resistance in preclinical data (86). However, this strategy did not show significant activity in a phase I/II trial in patients with acquired resistance to erlotinib (85). The new T790M specific inhibitor WZ-4002 is also under investigation, and has demonstrated to induce greater growth inhibition in vitro and in vivo against T790M than against WT EGFR (87). Indeed, the FLT3 inhibitor, an indolocarbazole compounds, is under investigation as potent and reversible inhibitor of EGFR T790M that spare wild-type EGFR in the context of T790M-mediated drug resistance in NSCLC (88).
Combined treatments of erlotinib plus therapies targeting compensatory pathways that lead to acquired EGFR TKI resistance may overcome resistance. The addition of a MET inhibitor may benefit those patients with EGFR mutant NSCLC and MET amplification. Antibodies targeting the MET ligand HGF (AMG102), MET itself (MetMAb), and small molecule inhibitors against MET are in clinical development. The combination of AXL inhibitors, such as XL880, MP-470 or SGI-7079, with an EGFR TKI is also a potential approach to overcome resistance associated with EMT (89).
Furthermore, inhibition of NOTCH-1 can be a novel strategy for the reversal of the EMT phenotype thereby potentially increasing therapeutic drug sensitivity to lung cancer cells. BEZ235, a dual inhibitor of PI3K and mTOR, would overcome EGFR-TKI resistance induced by HGF in an EGFR mutant lung cancer cell lines (90).
Finally, combination therapy with EGFR TKI and PI3KCA inhibitor, PARP inhibitors (in PTEN mutant patients), HER2 inhibitors, B-RAF inhibitors or IGFR inhibitors could have a therapeutic effect in tumors with acquired resistant to EGFR TKI by those mechanisms and some of them are being investigated in clinical trials (91).
Strategies to determine molecular basis of resistance to EGFR TKI in NSCLC with EGFR mutations
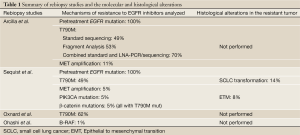
As commented previously, the biological basis underlying acquired EGFR TKI resistance is unknown in approximately 30% of patients. Some of these previously described mechanisms of resistance to EGFR TKI that have been identified in preclinical models and have not been validated in patients with acquired resistance. The analysis of clinical specimens is crucial to discover the remaining unknown mechanisms of EGFR TKI resistance. In the last years many authors have published their own experience with rebiopsies on patients with EGFR mutant NSCLC at the time of progression in order to identify how EGFR mutant NSCLC acquire resistance to EGFR TKI (Table 1).
Full Table
Arcila et al. undertook a rebiopsy study to determine the feasibility of rebiopsy in patients with EGFR mutant NSCLC with acquired resistance to EGFR TKI and to evaluate the spectrum of EGFR mutations and MET amplification in tumors at progression. One hundred and fifty three samples were obtained from 121 patients including frozen samples, fresh fluids, FFPE tissue and cytologies from fine needle aspirates (FNA); eighty-two per cent were successfully analyzed. Biopsies provided the highest success rate followed by FNA and pleural fluids. Pathologic confirmation was performed in 106 resistant tumors: one hundred and two adenocarcinomas, one squamous cell carcinoma, two small cell carcinomas and 1 with a mixed histology (combined large cell carcinoma/adenocarcinoma in one sample and a high grade neuroendocrine carcinoma in a second). EGFR mutations (exons 19 and 21) were found in 100/104 in resistant samples, seventy-one per cent had EGFR exon 19 deletions, one per cent had an insertion in exon 18 and 28% had an exon 21 point mutation. Of note, patients with multiple tissue sampling had the same mutation in all tumor sites, and all patients maintained the baseline sensitizing mutation. The T790M mutation was detected in 51% of mutant samples by standard analysis, and the retest of 30 negative patients by the LNA-PCR/sequencing method detected 11 additional mutants, raising the T790M mutation rate to 70%. MET amplification was found in 11% (4 patients), three of them also harbored the EGFR T790M mutation (57).
Sequist et al. performed rebiopsies on 37 EGFR mutant NSCLC patients with acquired resistance to identify the mechanisms of resistance to EGFR inhibitors. Pre- and post-EGFR TKI tumor samples were analyzed for the presence of genetic alterations with a genotyping platform (SNaPshot assay), and EGFR and MET amplification with fluorescence in situ hybridization (FISH). Eighteen (49%) patients acquired the T790M mutation, and two (5%) patients developed MET amplification, which was not present in the pretreatment specimen. Two (5%) patients showed acquired PIK3CA mutations, two (5%) cases had β-catenin mutations (together with the T790M mutation). Fifteen (41%) rebiopsies didn’t reveal any new mutations. The authors also found significant histological alterations in the resistant tumor; five patients (14%) had a diagnosis of SCLC, all maintaining the original EGFR mutation. Additionally, three resistant specimens had phenotypic changes consistent with a mesenchymal, supporting an ETM, none showed another identified resistance mechanism while maintained their original EGFR mutation. Of note, EMT or SCLC were not observed in biopsies from EGFR wild-type tumors resistant to chemotherapy (58).
Interestingly, multiple biopsies over the course of the disease were performed in 3 patients showing gain and loss of the T790M mutation in multiple biopsies from the same anatomical location during the clinical course in two of them at time of progression or when de EGFR TKI was interrupted. The rebiopsy from the third patient showed SCLC transformation with the original EGFR L858R mutation plus an acquired PIK3CA mutation. However, those changes were not observed at progression to treatment for SCLC, where adenocarcinoma histology with EGFR L858R mutation was again demonstrated (58). These results explain why retreatment of NSCLC patients with EGFR TKI who had experienced favorable results from their initial treatment could benefit some patients (53,92).
Oxnard et al. performed a rebiopsy protocol in EGFR mutant lung cancer patients with acquired resistance to EGFR TKI comparing for the presence of the T790M. T790M was identified in 62% of patients in the rebiopsy specimens with longer survival after progression than patients without T790M (49,59).
Finally, Ohashi et al. systematically screened for recurrent mutations in RAS/NRAS/BRAF/MEK1 in nearly 200 tumor samples from patients with acquired resistance to EGFR TKI. They found two BRAF mutations: one case with concurrent EGFR exon19 deletion and EGFR T790M and BRAF V600E mutations and another case with EGFR exon19 deletion and the BRAF G469A mutation (2/195, 1.0%). They studied further the biological and therapeutic consequences of acquired NRAS and BRAF mutations in EGFR-mutant lung tumor cells and showed that these tumor cells were resistant to erlotinib alone but were sensitive to combination treatment with EGFR and MEK inhibition (77).
There is no doubt that identifying the molecular mechanisms underlying variable response and resistance to EGFR TKI in EGFR mutant NSCLC is a major obstacle to optimize EGFR TKI therapy. A more comprehensive analysis of clinical specimens from EGFR TKI-treated patients should offer a better knowledge about if known mechanisms of resistance occur exclusively and concomitantly to promote clinical resistance. This is a key issue to resolve because we will need to determine whether to target individual or multiple drivers of resistance with targeted therapies in patients according to their molecular alterations present in their tumors.
Additionally, multiple rebiopsy studies also suggest that genetic mechanisms of resistance are potentially reversible, and therefore, a static diagnostic biopsy may be insufficient to guide therapeutic decision making throughout the course of a patient’s disease (58). To perform a rebiopsy at time of progression in EGFR mutant NSCLC patients is becoming more and more standard.
However, the underlying molecular basis of the heterogeneity in response to EGFR TKI has never been explored in patients immediately after initiation of therapy. This information would be crucial to study the early changes that can compromise response and progression and would help to uncover the molecular causes of treatment resistance and optimize the EGFR TKI therapy. Characterizing the complete molecular landscape of response to EGFR TKI in EGFR mutant NSCLC specimens from patients before and serially during treatment would reveal not only novel biomarkers of response to therapy but also potential new therapeutic targets to prevent or overcome resistance to EGFR TKI in NSCLC patients.
Summary
Several studies have showed that rebiopsy of EGFR mutant NSCLC patients with acquired resistance to EGFR TKI is feasible and provides sufficient material for mutation analysis in most patients. Interestingly, a wide heterogeneity in resistance mechanisms has been observed, each of which may require its own therapeutic strategy.
Indeed, it is becoming crucial the need of continuous assessment of each tumor evolution during the course of treatment not only to determine how it became resistant to therapy but also to allow us to design rational strategies to overcome resistance or to prevent acquired resistance in patients.
Since many patients do not undergo rebiopsy at progression, the lack of available resistant tumor tissue limits the molecular guided stratification of patients and negatively affects further investigation of acquired resistance. Of note, mechanisms of primary resistance are not usually analyzed in rebiopsy protocols in EGFR mutant NSCLC patients receiving EGFR TKI after the initiation of EGFR TKI which compromises a better understanding of how to prevent resistance to therapy.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Goldstraw P, Crowley J, Chansky K, et al. The IASLC Lung Cancer Staging Project: proposals for the revision of the TNM stage groupings in the forthcoming (seventh) edition of the TNM Classification of malignant tumours. J Thorac Oncol 2007;2:706-14. [PubMed]
- Mok TS, Wu YL, Thongprasert S, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med 2009;361:947-57. [PubMed]
- Paez JG, Jänne PA, Lee JC, et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science 2004;304:1497-500. [PubMed]
- Pao W, Miller V, Zakowski M, et al. EGF receptor gene mutations are common in lung cancers from “never smokers” and are associated with sensitivity of tumors to gefitinib and erlotinib. Proc Natl Acad Sci U S A 2004;101:13306-11. [PubMed]
- Rosell R, Moran T, Queralt C, et al. Screening for epidermal growth factor receptor mutations in lung cancer. N Engl J Med 2009;361:958-67. [PubMed]
- Mitsudomi T, Morita S, Yatabe Y, et al. Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised phase 3 trial. Lancet Oncol 2010;11:121-8. [PubMed]
- Rosell R, Carcereny E, Gervais R, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol 2012;13:239-46. [PubMed]
- Zhou C, Wu YL, Chen G, et al. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol 2011;12:735-42. [PubMed]
- Inoue A, Kobayashi K, Maemondo M, et al. Updated overall survival results from a randomized phase III trial comparing gefitinib with carboplatin-paclitaxel for chemo-naïve non-small cell lung cancer with sensitive EGFR gene mutations (NEJ002). Ann Oncol 2013;24:54-9. [PubMed]
- Lynch TJ, Bell DW, Sordella R, et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med 2004;350:2129-39. [PubMed]
- Sharma SV, Bell DW, Settleman J, et al. Epidermal growth factor receptor mutations in lung cancer. Nat Rev Cancer 2007;7:169-81. [PubMed]
- Maemondo M, Inoue A, Kobayashi K, et al. Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med 2010;362:2380-8. [PubMed]
- Mitsudomi T, Yatabe Y. Epidermal growth factor receptor in relation to tumor development: EGFR gene and cancer. FEBS J 2010;277:301-8. [PubMed]
- Wu JY, Wu SG, Yang CH, et al. Lung cancer with epidermal growth factor receptor exon 20 mutations is associated with poor gefitinib treatment response. Clin Cancer Res 2008;14:4877-82. [PubMed]
- Yasuda H, Kobayashi S, Costa DB. EGFR exon 20 insertion mutations in non-small-cell lung cancer: preclinical data and clinical implications. Lancet Oncol 2012;13:e23-31. [PubMed]
- Wu JY, Yu CJ, Chang YC, et al. Effectiveness of tyrosine kinase inhibitors on “uncommon” epidermal growth factor receptor mutations of unknown clinical significance in non-small cell lung cancer. Clin Cancer Res 2011;17:3812-21. [PubMed]
- Engelman JA, Zejnullahu K, Gale CM, et al. PF00299804, an irreversible pan-ERBB inhibitor, is effective in lung cancer models with EGFR and ERBB2 mutations that are resistant to gefitinib. Cancer Res 2007;67:11924-32. [PubMed]
- Li D, Ambrogio L, Shimamura T, et al. BIBW2992, an irreversible EGFR/HER2 inhibitor highly effective in preclinical lung cancer models. Oncogene 2008;27:4702-11. [PubMed]
- Yuza Y, Glatt KA, Jiang J, et al. Allele-dependent variation in the relative cellular potency of distinct EGFR inhibitors. Cancer Biol Ther 2007;6:661-7. [PubMed]
- Yun CH, Mengwasser KE, Toms AV, et al. The T790M mutation in EGFR kinase causes drug resistance by increasing the affinity for ATP. Proc Natl Acad Sci U S A 2008;105:2070-5. [PubMed]
- Kobayashi S, Boggon TJ, Dayaram T, et al. EGFR mutation and resistance of non-small-cell lung cancer to gefitinib. N Engl J Med 2005;352:786-92. [PubMed]
- Inukai M, Toyooka S, Ito S, et al. Presence of epidermal growth factor receptor gene T790M mutation as a minor clone in non-small cell lung cancer. Cancer Res 2006;66:7854-8. [PubMed]
- Girard N, Lou E, Azzoli CG, et al. Analysis of genetic variants in never-smokers with lung cancer facilitated by an Internet-based blood collection protocol: a preliminary report. Clin Cancer Res 2010;16:755-63. [PubMed]
- Bell DW, Gore I, Okimoto RA, et al. Inherited susceptibility to lung cancer may be associated with the T790M drug resistance mutation in EGFR. Nat Genet 2005;37:1315-6. [PubMed]
- Rosell R, Molina MA, Costa C, et al. Pretreatment EGFR T790M mutation and BRCA1 mRNA expression in erlotinib-treated advanced non-small-cell lung cancer patients with EGFR mutations. Clin Cancer Res 2011;17:1160-8. [PubMed]
- Rosell R, Molina-Vila M, Taron M, et al. EGFR compound mutants and survival on erlotinib in non-small cell lung cancer (NSCLC) patients (p) in the EURTAC study. J Clin Oncol 2012;30:abstr 7522.
- Fujita Y, Suda K, Kimura H, et al. Highly sensitive detection of EGFR T790M mutation using colony hybridization predicts favorable prognosis of patients with lung cancer harboring activating EGFR mutation. J Thorac Oncol 2012;7:1640-4. [PubMed]
- Balak MN, Gong Y, Riely GJ, et al. Novel D761Y and common secondary T790M mutations in epidermal growth factor receptor-mutant lung adenocarcinomas with acquired resistance to kinase inhibitors. Clin Cancer Res 2006;12:6494-501. [PubMed]
- Sos ML, Koker M, Weir BA, et al. PTEN loss contributes to erlotinib resistance in EGFR-mutant lung cancer by activation of Akt and EGFR. Cancer Res 2009;69:3256-61. [PubMed]
- Vivanco I, Rohle D, Versele M, et al. The phosphatase and tensin homolog regulates epidermal growth factor receptor (EGFR) inhibitor response by targeting EGFR for degradation. Proc Natl Acad Sci U S A 2010;107:6459-64. [PubMed]
- Kawano O, Sasaki H, Endo K, et al. PIK3CA mutation status in Japanese lung cancer patients. Lung Cancer 2006;54:209-15. [PubMed]
- Samuels Y, Wang Z, Bardelli A, et al. High frequency of mutations of the PIK3CA gene in human cancers. Science 2004;304:554. [PubMed]
- Engelman JA, Mukohara T, Zejnullahu K, et al. Allelic dilution obscures detection of a biologically significant resistance mutation in EGFR-amplified lung cancer. J Clin Invest 2006;116:2695-706. [PubMed]
- Gong Y, Yao E, Shen R, et al. High expression levels of total IGF-1R and sensitivity of NSCLC cells in vitro to an anti-IGF-1R antibody (R1507). PLoS One 2009;4:e7273. [PubMed]
- Sharma SV, Lee DY, Li B, et al. A chromatin-mediated reversible drug-tolerant state in cancer cell subpopulations. Cell 2010;141:69-80. [PubMed]
- Ben-Neriah Y, Karin M. Inflammation meets cancer, with NF-κB as the matchmaker. Nat Immunol 2011;12:715-23. [PubMed]
- Bivona TG, Hieronymus H, Parker J, et al. FAS and NF-κB signalling modulate dependence of lung cancers on mutant EGFR. Nature 2011;471:523-6. [PubMed]
- Akiyama T, Dass CR, Choong PF. Bim-targeted cancer therapy: a link between drug action and underlying molecular changes. Mol Cancer Ther 2009;8:3173-80. [PubMed]
- Wang Z, Zhang B, Yang L, et al. Constitutive production of NF-kappaB2 p52 is not tumorigenic but predisposes mice to inflammatory autoimmune disease by repressing Bim expression. J Biol Chem 2008;283:10698-706. [PubMed]
- Cragg MS, Kuroda J, Puthalakath H, et al. Gefitinib-induced killing of NSCLC cell lines expressing mutant EGFR requires BIM and can be enhanced by BH3 mimetics. PLoS Med 2007;4:1681-89; discussion 1690.
- Gong Y, Somwar R, Politi K, et al. Induction of BIM is essential for apoptosis triggered by EGFR kinase inhibitors in mutant EGFR-dependent lung adenocarcinomas. PLoS Med 2007;4:e294. [PubMed]
- Costa DB, Halmos B, Kumar A, et al. BIM mediates EGFR tyrosine kinase inhibitor-induced apoptosis in lung cancers with oncogenic EGFR mutations. PLoS Med 2007;4:1669-79; discussion 1680.
- Nakagawa T, Takeuchi S, Yamada T, et al. EGFR-TKI resistance due to BIM polymorphism can be circumvented by in combination with HDAC inhibition. Cancer Res 2013. [Epub ahead of print]. [PubMed]
- Carter TA, Wodicka LM, Shah NP, et al. Inhibition of drug-resistant mutants of ABL, KIT, and EGF receptor kinases. Proc Natl Acad Sci U S A 2005;102:11011-6. [PubMed]
- Majem M, Pallarès C. An update on molecularly targeted therapies in second- and third-line treatment in non-small cell lung cancer: focus on EGFR inhibitors and anti-angiogenic agents. Clin Transl Oncol 2013;15:343-57. [PubMed]
- Ramalingam SS, Blackhall F, Krzakowski M, et al. Randomized phase II study of dacomitinib (PF-00299804), an irreversible pan-human epidermal growth factor receptor inhibitor, versus erlotinib in patients with advanced non-small-cell lung cancer. J Clin Oncol 2012;30:3337-44. [PubMed]
- Pao W, Miller VA, Politi KA, et al. Acquired resistance of lung adenocarcinomas to gefitinib or erlotinib is associated with a second mutation in the EGFR kinase domain. PLoS Med 2005;2:e73. [PubMed]
- Chmielecki J, Foo J, Oxnard GR, et al. Optimization of dosing for EGFR-mutant non-small cell lung cancer with evolutionary cancer modeling. Sci Transl Med 2011;3:90ra59. [PubMed]
- Oxnard GR, Arcila ME, Sima CS, et al. Acquired resistance to EGFR tyrosine kinase inhibitors in EGFR-mutant lung cancer: distinct natural history of patients with tumors harboring the T790M mutation. Clin Cancer Res 2011;17:1616-22. [PubMed]
- Riely GJ, Kris MG, Zhao B, et al. Prospective assessment of discontinuation and reinitiation of erlotinib or gefitinib in patients with acquired resistance to erlotinib or gefitinib followed by the addition of everolimus. Clin Cancer Res 2007;13:5150-5. [PubMed]
- Milton DT, Riely GJ, Pao W, et al. Molecular on/off switch. J Clin Oncol 2006;24:4940-2. [PubMed]
- Kurata T, Tamura K, Kaneda H, et al. Effect of re-treatment with gefitinib (‘Iressa’, ZD1839) after acquisition of resistance. Ann Oncol 2004;15:173-4. [PubMed]
- Yano S, Nakataki E, Ohtsuka S, et al. Retreatment of lung adenocarcinoma patients with gefitinib who had experienced favorable results from their initial treatment with this selective epidermal growth factor receptor inhibitor: a report of three cases. Oncol Res 2005;15:107-11. [PubMed]
- Bean J, Riely GJ, Balak M, et al. Acquired resistance to epidermal growth factor receptor kinase inhibitors associated with a novel T854A mutation in a patient with EGFR-mutant lung adenocarcinoma. Clin Cancer Res 2008;14:7519-25. [PubMed]
- Costa DB, Schumer ST, Tenen DG, et al. Differential responses to erlotinib in epidermal growth factor receptor (EGFR)-mutated lung cancers with acquired resistance to gefitinib carrying the L747S or T790M secondary mutations. J Clin Oncol 2008;26:1182-4; author reply 1184-6. [PubMed]
- Engelman JA, Zejnullahu K, Mitsudomi T, et al. MET amplification leads to gefitinib resistance in lung cancer by activating ERBB3 signaling. Science 2007;316:1039-43. [PubMed]
- Arcila ME, Oxnard GR, Nafa K, et al. Rebiopsy of lung cancer patients with acquired resistance to EGFR inhibitors and enhanced detection of the T790M mutation using a locked nucleic acid-based assay. Clin Cancer Res 2011;17:1169-80. [PubMed]
- Sequist LV, Waltman BA, Dias-Santagata D, et al. Genotypic and histological evolution of lung cancers acquiring resistance to EGFR inhibitors. Sci Transl Med 2011;3:75ra26. [PubMed]
- Oxnard GR, Arcila ME, Chmielecki J, et al. New strategies in overcoming acquired resistance to epidermal growth factor receptor tyrosine kinase inhibitors in lung cancer. Clin Cancer Res 2011;17:5530-7. [PubMed]
- Bean J, Brennan C, Shih JY, et al. MET amplification occurs with or without T790M mutations in EGFR mutant lung tumors with acquired resistance to gefitinib or erlotinib. Proc Natl Acad Sci U S A 2007;104:20932-7. [PubMed]
- Suda K, Murakami I, Katayama T, et al. Reciprocal and complementary role of MET amplification and EGFR T790M mutation in acquired resistance to kinase inhibitors in lung cancer. Clin Cancer Res 2010;16:5489-98. [PubMed]
- Yano S, Wang W, Li Q, et al. Hepatocyte growth factor induces gefitinib resistance of lung adenocarcinoma with epidermal growth factor receptor-activating mutations. Cancer Res 2008;68:9479-87. [PubMed]
- Turke AB, Zejnullahu K, Wu YL, et al. Preexistence and clonal selection of MET amplification in EGFR mutant NSCLC. Cancer Cell 2010;17:77-88. [PubMed]
- Uramoto H, Yamada T, Yano S, et al. Prognostic value of acquired resistance-related molecules in Japanese patients with NSCLC treated with an EGFR-TKI. Anticancer Res 2012;32:3785-90. [PubMed]
- Suda K, Tomizawa K, Fujii M, et al. Epithelial to mesenchymal transition in an epidermal growth factor receptor-mutant lung cancer cell line with acquired resistance to erlotinib. J Thorac Oncol 2011;6:1152-61. [PubMed]
- Xie M, Zhang L, He CS, et al. Activation of Notch-1 enhances epithelial-mesenchymal transition in gefitinib-acquired resistant lung cancer cells. J Cell Biochem 2012;113:1501-13. [PubMed]
- Shan B, Yao TP, Nguyen HT, et al. Requirement of HDAC6 for transforming growth factor-beta1-induced epithelial-mesenchymal transition. J Biol Chem 2008;283:21065-73. [PubMed]
- Serizawa M, Takahashi T, Yamamoto N, et al. Combined Treatment with Erlotinib and a Transforming Growth Factor-β Type I Receptor Inhibitor Effectively Suppresses the Enhanced Motility of Erlotinib-Resistant Non-Small-Cell Lung Cancer Cells. J Thorac Oncol 2013;8:259-69. [PubMed]
- Morgillo F, Cascone T, D’Aiuto E, et al. Antitumour efficacy of MEK inhibitors in human lung cancer cells and their derivatives with acquired resistance to different tyrosine kinase inhibitors. Br J Cancer 2011;105:382-92. [PubMed]
- Yauch RL, Januario T, Eberhard DA, et al. Epithelial versus mesenchymal phenotype determines in vitro sensitivity and predicts clinical activity of erlotinib in lung cancer patients. Clin Cancer Res 2005;11:8686-98. [PubMed]
- Coldren CD, Helfrich BA, Witta SE, et al. Baseline gene expression predicts sensitivity to gefitinib in non-small cell lung cancer cell lines. Mol Cancer Res 2006;4:521-8. [PubMed]
- Zhang Z, Lee JC, Lin L, et al. Activation of the AXL kinase causes resistance to EGFR-targeted therapy in lung cancer. Nat Genet 2012;44:852-60. [PubMed]
- Yamamoto C, Basaki Y, Kawahara A, et al. Loss of PTEN expression by blocking nuclear translocation of EGR1 in gefitinib-resistant lung cancer cells harboring epidermal growth factor receptor-activating mutations. Cancer Res 2010;70:8715-25. [PubMed]
- Mendes-Pereira AM, Martin SA, Brough R, et al. Synthetic lethal targeting of PTEN mutant cells with PARP inhibitors. EMBO Mol Med 2009;1:315-22. [PubMed]
- Takezawa K, Pirazzoli V, Arcila ME, et al. HER2 amplification: a potential mechanism of acquired resistance to EGFR inhibition in EGFR-mutant lung cancers that lack the second-site EGFRT790M mutation. Cancer Discov 2012;2:922-33. [PubMed]
- Blakely CM, Bivona TG. Resiliency of lung cancers to EGFR inhibitor treatment unveiled, offering opportunities to divide and conquer EGFR inhibitor resistance. Cancer Discov 2012;2:872-5. [PubMed]
- Ohashi K, Sequist LV, Arcila ME, et al. Lung cancers with acquired resistance to EGFR inhibitors occasionally harbor BRAF gene mutations but lack mutations in KRAS, NRAS, or MEK1. Proc Natl Acad Sci U S A 2012;109:E2127-33. [PubMed]
- Harada D, Takigawa N, Ochi N, et al. JAK2-related pathway induces acquired erlotinib resistance in lung cancer cells harboring an epidermal growth factor receptor-activating mutation. Cancer Sci 2012;103:1795-802. [PubMed]
- Guix M, Faber AC, Wang SE, et al. Acquired resistance to EGFR tyrosine kinase inhibitors in cancer cells is mediated by loss of IGF-binding proteins. J Clin Invest 2008;118:2609-19. [PubMed]
- Tabara K, Kanda R, Sonoda K, et al. Loss of activating EGFR mutant gene contributes to acquired resistance to EGFR tyrosine kinase inhibitors in lung cancer cells. PLoS One 2012;7:e41017. [PubMed]
- Kwak EL, Sordella R, Bell DW, et al. Irreversible inhibitors of the EGF receptor may circumvent acquired resistance to gefitinib. Proc Natl Acad Sci U S A 2005;102:7665-70. [PubMed]
- Sequist LV, Besse B, Lynch TJ, et al. Neratinib, an irreversible pan-ErbB receptor tyrosine kinase inhibitor: results of a phase II trial in patients with advanced non-small-cell lung cancer. J Clin Oncol 2010;28:3076-83. [PubMed]
- Miller VA, Hirsh V, Cadranel J, et al. Afatinib versus placebo for patients with advanced, metastatic non-small-cell lung cancer after failure of erlotinib, gefitinib, or both, and one or two lines of chemotherapy (LUX-Lung 1): a phase 2b/3 randomised trial. Lancet Oncol 2012;13:528-38. [PubMed]
- Regales L, Gong Y, Shen R, et al. Dual targeting of EGFR can overcome a major drug resistance mutation in mouse models of EGFR mutant lung cancer. J Clin Invest 2009;119:3000-10. [PubMed]
- Janjigian YY, Azzoli CG, Krug LM, et al. Phase I/II trial of cetuximab and erlotinib in patients with lung adenocarcinoma and acquired resistance to erlotinib. Clin Cancer Res 2011;17:2521-7. [PubMed]
- Wang M, Zhao J, Zhang LM, et al. Combined Erlotinib and Cetuximab overcome the acquired resistance to epidermal growth factor receptors tyrosine kinase inhibitor in non-small-cell lung cancer. J Cancer Res Clin Oncol 2012;138:2069-77. [PubMed]
- Zhou W, Ercan D, Chen L, et al. Novel mutant-selective EGFR kinase inhibitors against EGFR T790M. Nature 2009;462:1070-4. [PubMed]
- Lee HJ, Schaefer G, Heffron TP, et al. Noncovalent Wild-type-Sparing Inhibitors of EGFR T790M. Cancer Discov 2013;3:168-81. [PubMed]
- Byers LA, Diao L, Wang J, et al. An epithelial-mesenchymal transition gene signature predicts resistance to EGFR and PI3K inhibitors and identifies Axl as a therapeutic target for overcoming EGFR inhibitor resistance. Clin Cancer Res 2013;19:279-90. [PubMed]
- Sano T, Takeuchi S, Nakagawa T, et al. The novel phosphoinositide 3-kinase-mammalian target of rapamycin inhibitor, BEZ235, circumvents erlotinib resistance of epidermal growth factor receptor mutant lung cancer cells triggered by hepatocyte growth factor. Int J Cancer 2013;133:505-13. [PubMed]
- Gadgeel SM, Wozniak A. Preclinical Rationale for PI3K/Akt/mTOR Pathway Inhibitors as Therapy for Epidermal Growth Factor Receptor Inhibitor-Resistant Non-Small-Cell Lung Cancer. Clin Lung Cancer 2013. [Epub ahead of print]. [PubMed]
- Yoshimoto A, Inuzuka K, Kita T, et al. Remarkable effect of gefitinib retreatment in a patient with nonsmall cell lung cancer who had a complete response to initial gefitinib. Am J Med Sci 2007;333:221-5. [PubMed]


