
18F-fluorodeoxyglucose positron emission tomography/computed tomography in the diagnosis of benign pulmonary lesions in sarcoidosis
Introduction
18F-fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) has been shown to be an accurate, noninvasive imaging modality for differentiating benign from malignant pulmonary lesions. Compared with classical methods of imaging, a PET/CT scan shows not only the morphology but also the metabolism of the suspicious lesions.
However, increased uptake of 18F-FDG may also represent nonneoplastic infectious lesions, which is connected with excessive activity of macrophages and neutrophils in the tissues (1). Some of the benign lung lesions may appear as false positives, because 18F-FDG is nonspecific tumor imaging agent. If the morphological appearance of the lesion is not typical, it can be difficult to diagnose, and there may be the possibility of the misdiagnosis of lung cancer.
The objective of this study was to analyze the uptake characteristics of benign pulmonary lesions on 18F-FDG PET/CT imaging and to assess the usefulness of PET/CT in the evaluation of benign pulmonary lesions to improve the diagnosis and differential diagnosis of benign pulmonary lesions.
Methods
Patients
This study was approved by the Institutional Ethics Board of Jinling Hospital (No. DBNJ005), and the requirement for patient informed consent was waived.
Patients with pulmonary nodules or masses referred to Jinling Hospital for 18F-FDG PET/CT imaging from January 2010 to May 2017 were retrospectively evaluated.
The study group included 113 patients (75 men and 38 women). All cases were proven to be benign pulmonary lesions by pathology or diagnostic therapy. Histological or cytological examination of the biopsy specimens obtained from bronchoscopy and percutaneous lung puncture was performed.
18F-FDG PET/CT imaging acquisition
18F-FDG PET/CT images were obtained using a Discovery ST PET/CT scanner (General Electric, USA) equipped with high-resolution bismuth germinate detectors and a 16-slice CT scanner. All patients fasted for at least 6 h before 18F-FDG PET/CT examinations, and their blood glucose was documented as below 8 mmol/L before receiving the 18F-FDG injection. According to weight, the patients received intravenous injections of the imaging agent 18F-FDG 3.70–4.44 MBq/kg. A low-dose unenhanced CT scan was performed before PET imaging to provide attenuation correction by a standard protocol using 120 kV, 150 mAs, a tube-rotation time of 0.8 s per rotation, and a pitch of 3.75 mm. The cross-sectional sinogram data were corrected for dead time, decay, random coincidences, and attenuation.
Image analysis
The uptake of 18F-FDG in lesions was based on semiquantitative analysis and the visual comparison method to make a comprehensive judgment. Semiquantitative analysis was performed by using the maximum standardized uptake value (SUVmax) corrected by lean body mass (LBM).
The specific method was to set the region of interest (ROI) at the location of the lung lesions. The system automatically measured the SUVmax of the lesions. The size of the lesion was expressed by maximum diameter (2).
Statistical analysis
SPSS 22.0 software (SPSS, Inc., Chicago, IL, USA) was used for all analyses. The data of the continuous variables were expressed as mean ± SD. ANOVA single factor variance analysis and the Kruskal-Wallis test were used to compare the uptake of different pathological lesions. Pairwise comparison of the areas under receiver operating characteristic (ROC) curves (AUC) for the parameters used to diagnose sarcoidosis lesions was made to determine significant differences. The determination of cut-off values was based on an acceptable value of sensitivity (>80%) and the Youden index in ROC analysis, which is the sum of sensitivity and specificity minus 1 (3). A P value less than 0.05 was considered to indicate a statistically significant difference.
Results
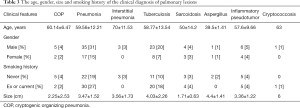
One hundred and thirteen patients (75 men and 38 women) with benign pulmonary lesions, whose mean age was 58.57±12.85 years, were evaluated. The average diameter of the 113 pulmonary lesions was 3.49±1.84 cm (range, 0.14–10.8 cm), and they were measured along their greatest diameter for the CT images. According to its pathological type, pulmonary lesions can be divided into two broad categories: inflammatory lesions and granulomatous lesions. There were 77 cases of inflammatory lesions and 36 cases of granulomatous lesions. The values of SUVmax were significantly higher in granulomatous lesions compared with inflammatory pulmonary lesions, while age, gender, size, average diameter and smoking history did not reflect such differences (Table 1).

Full table
The histopathologic diagnoses subcategories of the 113 lesions are shown in Table 2. Neutrophil-based inflammation was the most common inflammatory lesion (38/77, 49%), and tuberculosis was the most common granulomatous lesion (25/36, 69%). There were 24 lymphocytic-based lesions, accounting for 21% of the total. In the inflammatory lesions, the values for SUVmax of the lesions with neutrophil-based inflammation were significantly higher than that of the lesions with lymphocytic-based inflammation (5.81±2.37 vs. 2.03±1.57).

Full table
We conducted further investigation and follow-up of the cases. Each patient had been given a clinical diagnosis. The clinical diagnosis classifications of the 113 lesions are shown in Table 3. Pneumonia was the most common inflammatory lesion (52/113, 46%), and tuberculosis was the most common granulomatous lesion (31/113, 27%). Patients with cryptococcosis and cryptococcosis were the least common, both with only 1 case (1%). The average age of the patients with interstitial pneumonia was the oldest (70±11.53 years).
Full table
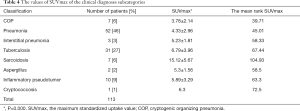
The values of uptake of 18F-FDG of the clinical diagnoses subcategories are shown in Table 4. In the clinical diseases, the SUVmax of sarcoidosis was significantly higher than that other types of diseases (15.12±5.67). The second highest values were for tuberculosis and cryptococcosis (6.79±3.96; 6.3), respectively. However, cryptococcosis had only one case and could not reflect the general trend.
Full table
Discussion
Previous studies have demonstrated the value of 18F-FDG PET/CT in characterization of lung lesions (4,5), and in the study by Fletcher et al., the diagnostic sensitivity and specificity of 18F-FDG PET for lung cancer could reach 91.7% and 82.3%, respectively, in a cohort of 344 patients (5). However, some studies suggested that the value of 18F-FDG PET/CT in evaluating lung lesions had been overestimated (6), especially in the solitary pulmonary nodules (SPNs), and its diagnostic sensitivity did not exceed 70% in characterizing SPNs (6,7). Nonsolid cancerous nodules, which typically exhibit slow-growth characteristics, are liable to be mistakenly diagnosed as benign lesions by 18F-FDG PET (8-12). The SUVmax threshold of 2.5, when used for diagnosing malignant solitary pulmonary lesions in some previous studies, was found to retain a high sensitivity (97%); however, the specificity was low (38%) (13,14). The 18F-FDG uptake in inflammatory nodules, tuberculosis and other granulomatous lesions can also be very high. Rogers et al. (15) found the metabolism of inflammatory cells, such as macrophages, lymphocytes and granulocytes, sharply increased demand for glucose and the expression of glucose transporters, resulting in more 18F-FDG uptake. The characteristics of 18F-FDG uptake on 18F-FDG PET/CT are important to diagnose benign pulmonary lesions, so we can avoid misdiagnosis and give patients better treatment.
This study assessed the values of 18F-FDG uptake in benign pulmonary lesions with histopathologic diagnoses and clinical diagnoses. According to its pathological type, pulmonary lesions can be divided into two broad categories: inflammatory lesions and granulomatous lesions. We found the values of 18F-FDG uptake were significantly higher in granulomatous pulmonary lesions compared with inflammatory pulmonary lesions in our study. Davis et al. (16) found that the degree of aggregation of 18F-FDG was related to the degree of inflammatory activity; active pulmonary tuberculosis was characterized by high intake, but after treatment or resolution of pulmonary tuberculosis, there was no apparent uptake or moderate uptake. The 18F-FDG uptake in tuberculosis was high, especially for studies performed in tuberculosis-endemic regions (17). This is consistent with our findings. In our subgroup analysis of histopathological groups, tuberculosis was in the majority, and tuberculosis and fungus had higher values of 18F-FDG uptake. However, the SUVmax of the lesions with neutrophil-based inflammation was significantly higher than that of lymphocytic-based inflammation. According to these studies (and also based on our data), we inferred that the metabolism of neutrophil-based inflammation was more active than the metabolism of lymphocytic-based inflammation.
Is the size of benign pulmonary lesions related to the uptake of 18F-FDG? Hara et al. (18) reported that SUVmax was positively correlated with the size of tuberculosis lesions. Lee et al. (19) analyzed ten cases of pulmonary sclerosing hemangioma (PSH), and they concluded there was a positive correlation between the uptake of the lesions (SUVmax) and lesion size. In our study, we found no statistically significant correlation between lesion size and SUVmax. We concluded it probably was because most of the patients in our group had large lesions, as the mean maximum diameter of the lesions was 3.49±1.84. Large lesions probably contain more active cells than small lesions, and their uptake is also higher.
We conducted further investigation and follow-up of the cases and evaluated SUVmax in the clinical diagnostic groups. We found the SUVmax of sarcoidosis was highest in all the types of diseases (15.12±5.67). The second highest values were in tuberculosis and cryptococcosis (6.79±3.96; 6.3), respectively. The data analysis showed that the SUVmax of sarcoidosis was useful for discriminating between other pulmonary benign lesions. Sarcoidosis is characterized by the formation of noncaseating granulomas in multiple organ systems and is associated with symptoms such as dyspnea, low-grade fever, weight loss, skin rashes, and vision changes (20). In the study by Treglia et al., 18F-FDG-PET/CT appeared to be useful for staging, evaluating disease activity, and monitoring treatment responses in patients with sarcoidosis (21). Our study found that 18F-FDG-PET/CT plays a differential role in the diagnosis of sarcoidosis. Furthermore, the SUVmax of 2.5 (delayed SUVmax of more than 2.5) was used as the traditional threshold for diagnosing malignant pulmonary lesions (13,22). In our study, all the lesions were benign, but the SUVmax was generally higher than the threshold of 2.5. According to those studies (and also based on our data), we inferred that a SUVmax threshold of 2.5 seemed inadequate for determining the nature of pulmonary lesions due to its low specificity; therefore, a higher cut-off value was needed.
Our study had several limitations including its small sample size and selection bias, since this was a retrospective study and enrolled only patients with pathologically proven pulmonary lesions. In addition, we did not use the delayed scan to compare early and delayed SUVs, although Cheng found that delayed 18F-FDG PET imaging may lead to easier detection of either malignant or benign lesions (23). Future studies are required to evaluate the efficacy of 18F-FDG PET/CT imaging in delineating the subgroups of pulmonary lesions.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the Institutional Ethics Board of Jinling Hospital (No. DBNJ005), and the requirement for patient informed consent was waived.
References
- Bakheet SM, Saleem M, Powel J, et al. F-18 fluorodeoxyglucose chest uptake in lung inflammation and infection. Clin Nucl Med 2000;25:273-8. [Crossref] [PubMed]
- Zhou WL, Wu HB, Wang LJ, et al. Usefulness and pitfalls of F-18-FDG PET/CT for diagnosing extramedullary acute leukemia. Eur J Radiol 2016;85:205-10. [Crossref] [PubMed]
- Schisterman EF, Perkins NJ, Liu A, et al. Optimal cut-point and its corresponding Youden Index to discriminate individuals using pooled blood samples. Epidemiology 2005;16:73-81. [Crossref] [PubMed]
- Bar-Shalom R, Kagna O, Israel O, et al. Noninvasive diagnosis of solitary pulmonary lesions in cancer patients based on 2-fluoro-2-deoxy-D-glucose avidity on positron emission tomography/computed tomography. Cancer 2008;113:3213-21. [Crossref] [PubMed]
- Fletcher JW, Kymes SM, Gould M, et al. A comparison of the diagnostic accuracy of 18F-FDG PET and CT in the characterizatio of solitary pulmonary nodules. J Nucl Med 2008;49:179-85. [Crossref] [PubMed]
- Li S, Zhao B, Wang X, et al. Overestimated value of (18)F-FDG PET/ CT to diagnose pulmonary nodules: analysis of 298 patients. Clin Radiol 2014;69:e352-7. [Crossref] [PubMed]
- van Gómez López O, García Vicente AM, Honguero Martínez AF, et al. (18)F-FDG-PET/CT in the assessment of pulmonary solitary nodules: comparison of different analysis methods and risk variables in the prediction of malignancy. Transl Lung Cancer Res 2015;4:228-35. [PubMed]
- Lee HY, Lee KS. Ground-glass opacity nodules: histopathology, imaging evaluation, and clinical implications. J Thorac Imaging 2011;26:106-18. [Crossref] [PubMed]
- Raad RA, Suh J, Harari S, et al. Nodule characterization: subsolid nodules. Radiol Clin North Am 2014;52:47-67. [Crossref] [PubMed]
- Seidelman JL, Myers JL, Quint LE. Incidental, subsolid pulmonary nodules at CT:etiology and management. Cancer Imaging 2013;13:365-73. [Crossref] [PubMed]
- Lee HY, Choi YL, Lee KS, et al. Pure ground-glass opacity neoplastic lung nodules: histopathology, imaging, and management. AJR Am J Roentgenol 2014;202:W224-33. [Crossref] [PubMed]
- Ambrosini V, Nicolini S, Caroli P, et al. PET/CT imaging in different types of lung cancer:an overview. Eur J Radiol 2012;81:988-1001. [Crossref] [PubMed]
- Al-Sugair A, Coleman RE. Applications of PET in lung Cancer. Semin Nucl Med 1998;28:303-19. [Crossref] [PubMed]
- Huang YE, Huang YJ, Ko M, et al. Dual-time-point 18F-FDG PET/CT in the diagnosis of solitary pulmonary lesions in a region with endemic granulomatous diseases. Ann Nucl Med 2016;30:652-8. [Crossref] [PubMed]
- Rogers S, Macheda ML, Docherty SE, et al. Identification of a novel glucose transporter-like protein-GLUT-12. Am J Physiol Endocrinol Metab 2002;282:E733-8. [Crossref] [PubMed]
- Davis SL, Nuermberger EL, Um PK, et al. Noninvasive pulmonary (18F)-2-fluoro-deoxy-D-glucose positron emission tomography correlates with bactericidal activity of tuberculosis drug treatment. Antimicrob Agents Chemother 2009;53:4879-84. [Crossref] [PubMed]
- Zheng Z, Pan Y, Guo F, et al. Multimodality FDG PET/CT appearance of pulmonary tuberculoma mimicking lung cancer and pathologic correlation in a tuberculosis-endemic country. South Med J 2011;104:440-5. [Crossref] [PubMed]
- Hara T, Kosaka N, Suzuki T, et al. Uptake rates of 18Ffluorodeoxyglucose and 11C-choline in lung cancer and pulmonary tuberculosis: a positron emission tomography study. Chest 2003;124:893-901. [Crossref] [PubMed]
- Lee E, Park CM, Kang KW, et al. 18F-FDG PET/CT features of pulmonary sclerosing hemangioma. Acta Radiol 2013;54:24-9. [Crossref] [PubMed]
- Heinle R, Chang C. Diagnostic criteria for sarcoidosis. Autoimmun Rev 2014;13:383-7. [Crossref] [PubMed]
- Treglia G, Annunziata S, Sobic-Saranovic D, et al. The role of 18F-FDG-PET and PET/CT in patients with sarcoidosis: an updated evidence-based review. Acad Radiol 2014;21:675-84. [Crossref] [PubMed]
- Macdonald K, Searle J, Lyburn I. The role of dual time point FDG PET imaging in the evaluation of solitary pulmonary nodules with an initial standard uptake value less than 2.5. Clin Radiol 2011;66:244-50. [Crossref] [PubMed]
- When should we recommend use of dual time-point and delayed time-point imaging techniques in FDG PET? Eur J Nucl Med Mol Imaging 2013;40:779-87. [Crossref] [PubMed]


